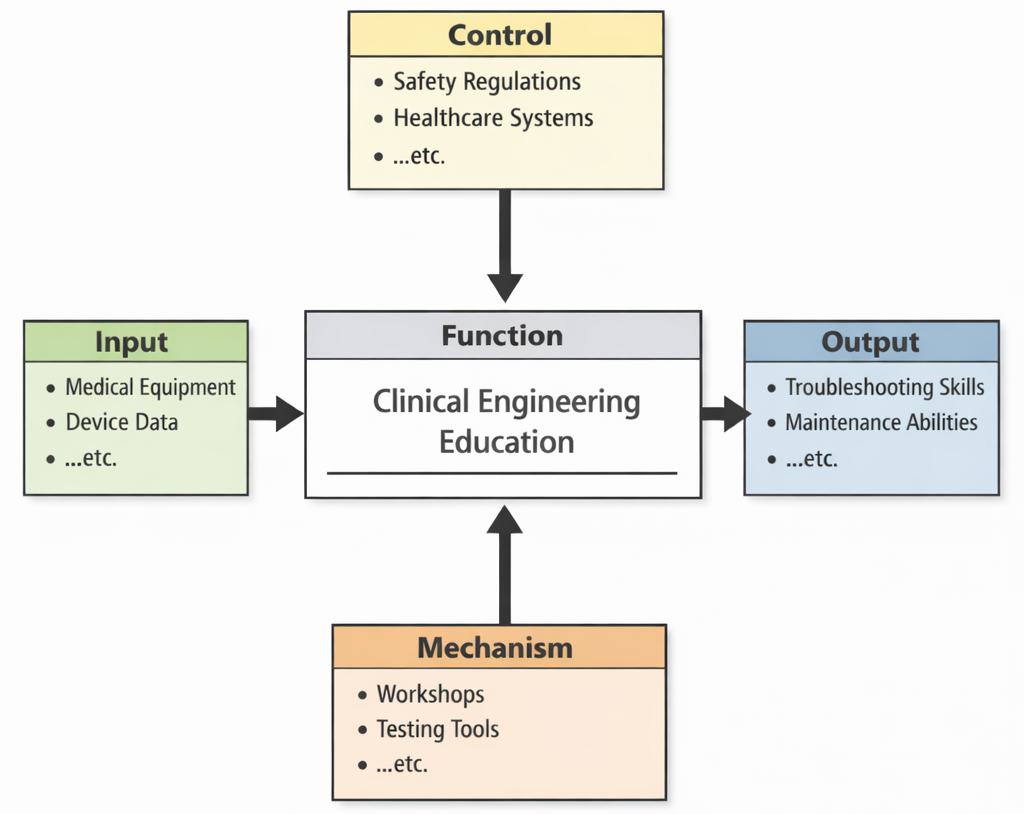
Clinical Engineering Education, as depicted in this IDEF0 diagram, functions as a practical transformation process that turns real hospital device Inputs into dependable professional capability. Students begin with Inputs such as medical equipment and device data—the physical systems, performance readings, alarms, logs, and maintenance histories that define day-to-day clinical technology work. Their learning is shaped by Controls like safety regulations and healthcare systems, which act as the non-negotiable guardrails: devices must meet safety requirements, fit clinical workflows, and support patient care without creating hidden risks. The transformation is enabled by Mechanisms such as workshops and testing tools, where learners practice inspection, calibration, verification, fault isolation, documentation, and communication with clinical teams. The Outputs are the core outcomes shown on the right: troubleshooting skills and maintenance abilities—meaning graduates can keep equipment reliable, diagnose failures systematically, prevent downtime, and ensure that technology in healthcare remains safe, compliant, and ready when patients need it most.
Clinical Engineering is a specialized branch of Biomedical Engineering that bridges the gap between medical technology and patient care. Professionals in this field are responsible for ensuring that complex healthcare technologies are properly designed, maintained, and integrated into clinical settings. Through the application of tools developed in Bioinformatics, engineers can manage large volumes of clinical data to optimize equipment functionality and track patient outcomes.
The reliability of medical devices often depends on advanced materials sourced from Biomaterials, which offer the biocompatibility and mechanical strength needed for safe implementation. Clinical engineers must also understand human movement and loading conditions—topics central to Biomechanics—to support the design of assistive devices and rehabilitation systems. Increasingly, diagnostic monitoring through Biomedical Signal Processing enables proactive maintenance of both patient-monitoring tools and therapy devices.
Heart-related devices such as pacemakers and ventricular assist devices require close collaboration with experts in Cardiovascular Engineering, while image-guided procedures rely on technology derived from Medical Imaging. Engineers also draw upon insights from Neural Engineering to manage devices interfacing with the nervous system. In the realm of drug delivery, Pharmaceutical Engineering ensures compatibility between pharmaceuticals and their delivery mechanisms.
Post-operative and rehabilitative technology depends on collaboration with Rehabilitation Engineering, especially in configuring mobility aids and prosthetic integration. For longer-term innovations, fields like Tissue Engineering and Regenerative Medicine inspire devices for growing or repairing biological tissues. Cross-disciplinary collaboration also extends to Chemical Engineering when designing biosensors and sterilization protocols.
Engineers apply concepts from Biochemical Engineering to manage the safe disposal of biohazardous substances. In developing reaction-based diagnostics, Chemical Catalysis and Reaction Engineering plays a key role. Energy systems used to power mobile medical units benefit from contributions by Chemical Energy Systems Engineering.
Material robustness in clinical settings is informed by Chemical Materials Engineering, while process optimization of sterilization units can be enhanced using Chemical Process Engineering. Sophisticated system simulations are often supported by Computational Chemical Engineering, especially for virtual prototyping. Clinical hygiene procedures sometimes adopt food-safe standards modeled from Food and Beverage Engineering.
The use of nanomaterials in monitoring and targeted therapy draws from Nanotechnology in Chemical Engineering. Material selection for single-use and reusable clinical tools is guided by Polymer and Plastics Engineering. Infrastructure-level planning for healthcare facilities engages principles from Civil Engineering, and operational logistics occasionally borrow insights from Construction Management. Furthermore, emergency technology deployment in hospitals aligns with methodologies in Earthquake and Disaster Engineering, emphasizing safety and resilience.

This illustration presents clinical engineering as the “behind-the-scenes” discipline that makes modern healthcare technology work smoothly. At the center is a major imaging machine (MRI/CT-style) with a patient positioned for scanning, symbolizing high-value equipment that requires careful setup, calibration, and maintenance. A clinical engineer in the foreground reviews data on a tablet, suggesting performance checks, troubleshooting, and safety documentation. Around the room are carts, instruments, and staff, highlighting workflow, device integration, and day-to-day support in clinical environments. The lower panels with waveform monitors and scan readouts emphasize quality assurance, testing, and continual monitoring—core responsibilities of clinical engineers who ensure devices meet standards, remain dependable, and protect patients and healthcare teams.
- Biomedical Engineering topics:
- Biomedical Engineering – Overview
- Biomechanics
- Biomaterials
- Tissue Engineering & Regenerative Medicine
- Cardiovascular Engineering
- Neural Engineering
- Medical Imaging
- Biomedical Signal Processing
- Bioinformatics
- Pharmaceutical Engineering
- Rehabilitation Engineering
- Clinical Engineering
Table of Contents
Core Functions of Clinical Engineering
1. Medical Equipment Management
- Procurement and Evaluation:
- Clinical engineers conduct needs assessments by collaborating with physicians, nurses, and administrators to identify gaps in medical infrastructure and equipment.
- They evaluate devices based on performance, total cost of ownership, lifecycle support, interoperability, and clinical impact.
- Structured procurement protocols are established to ensure transparency, vendor accountability, and adherence to institutional budgets.
- Health technology assessments (HTAs) involve analyzing safety data, clinical trial results, and cost-benefit models to inform evidence-based purchasing decisions.
- Installation and Commissioning:
- Engineers oversee the safe delivery and physical setup of equipment, ensuring structural compatibility, power supply, and environmental requirements (e.g., MRI shielding).
- They perform calibration checks, baseline performance measurements, and accuracy verifications in line with manufacturers’ specifications.
- Commissioning involves generating detailed test reports and functional validation to meet regulatory standards and internal quality benchmarks.
- Maintenance and Repairs:
- Routine inspections and preventive maintenance plans are scheduled based on risk stratification, usage frequency, and device criticality.
- Performance metrics such as downtime, mean time between failure (MTBF), and cost per user session are tracked and analyzed.
- Prompt corrective action is taken for malfunctioning devices, including parts replacement, sensor recalibration, or software updates.
- A centralized asset management system tracks maintenance history, service logs, warranty coverage, and replacement timelines.
2. Equipment Safety and Compliance
- Regulatory Compliance:
- Clinical engineers ensure devices are CE‑marked, FDA‑cleared, or registered under other recognized authorities.
- They maintain up-to-date documentation for ISO 13485, IEC 60601, and local regulatory mandates.
- Vigilance programs are implemented to report adverse events and track field safety notices and recalls.
- Risk Management:
- Engineers use failure mode and effects analysis (FMEA), root cause analysis (RCA), and risk registers to manage hazard control.
- They lead periodic safety audits, including electrical safety tests and software cybersecurity checks.
- Recall management includes quarantining unsafe equipment, coordinating with vendors, and communicating corrective instructions to clinical teams.
3. Technology Integration and Clinical Support
- System Integration:
- Clinical engineers integrate medical devices (e.g., patient monitors, infusion pumps, lab analyzers) with EHR and HIS systems via HL7, FHIR, or DICOM protocols.
- They manage middleware platforms and interface engines to ensure seamless data exchange and interoperability.
- Secure network architecture and encrypted data workflows are designed to prevent unauthorized access and comply with HIPAA/GDPR.
- Clinical Collaboration:
- Engineers support clinical procedures involving complex equipment (e.g., MRIs, CT scanners, robotic surgical systems).
- They attend rounds, offer on-call technical assistance, and optimize device utilization workflows.
- Engineers participate in multidisciplinary practice committees, offering input on device selection and technical feasibility assessments.
4. Training and Education
- Staff Training:
- Clinical engineers design structured training programs for nurses, technicians, and physicians on safe device handling and troubleshooting.
- They facilitate practical training sessions, competency assessments, and continuing education modules.
- Simulated scenarios are used to prepare clinical staff for emergency protocols, such as malfunction of ventilators or defibrillators.
- User Manuals and Protocols:
- Engineers develop SOPs, quick-reference cards, and vendor support guides tailored to institutional protocols.
- Visual aids such as infographics and embedded tutorial videos improve user comprehension and adoption.
- Regular revision of documentation ensures compliance with updated device firmware and institutional policies.
5. Research and Innovation
- Technology Assessment:
- Engineers monitor emerging technologies—augmented reality surgical systems, AI diagnostics, wearable monitors—and evaluate clinical readiness.
- They conduct pilot studies to measure performance, cost implications, and patient outcomes.
- Findings inform evidence-based adoption strategies and ROI analysis for institutional investment.
- Custom Device Development:
- Collaborating with biomedical engineering teams, clinical engineers prototype bespoke solutions—such as safety locks for infusion pumps or custom sensor mounts.
- They coordinate with regulatory bodies to validate changes in safety profiles, usability, and traceability.
- Rapid prototyping—using 3D printing, microcontrollers, or embedded software—enables agile development and real-world testing.
6. Strategic Management and Policy
- Engineers advise hospital leadership on capital planning, cost-benefit analyses, and service-level agreements (SLAs) with vendors.
- They develop performance dashboards to monitor asset utilization, maintenance costs, and risk exposure.
- Strategic plans align technical services with institutional goals such as patient safety, accreditation readiness, and digital transformation.
7. Emergency Preparedness and Resilience
- Clinical engineers develop continuity plans to maintain critical equipment functionality during disasters, cyberattacks, or pandemics.
- They manage backup power systems, mobile diagnostic units, and rapid equipment redistribution protocols.
- Regular drills simulate failure modes and emergency repairs to strengthen organizational resilience.
8. Data Analytics and Performance Optimization
- Engineers analyze maintenance logs and asset performance to identify failure patterns and predict maintenance needs.
- Machine learning models estimate device degradation, enabling preventive interventions before failures occur.
- Analytics dashboards provide real-time insights into equipment usage trends and cost per procedure.
External Resources
- AAMI – Standards and Guidelines for Medical Device Management
- FDA – Medical Device Regulation and Compliance
- HIMSS – Clinical Engineering Resources
- PMC – Clinical Engineering in Healthcare: A Review
- ISO – Technical Committee ISO/TC 210 on Quality Management and IMDRF
Key Areas of Clinical Engineering
Medical Equipment Lifecycle Management
- Planning:
- Assessing clinical needs and creating procurement plans aligned with healthcare goals.
- Acquisition:
- Vendor negotiations, budget management, and technology assessments.
- Deployment:
- Ensuring correct installation and user acceptance testing (UAT).
- Maintenance:
- Scheduling routine inspections and calibrations.
- Disposal:
- Environmentally responsible decommissioning of obsolete equipment.
Hospital Infrastructure and Facilities
- Critical Care Systems:
- Managing systems such as medical gas supply, ventilators, and life-support devices.
- Operating Rooms and Intensive Care Units:
- Ensuring the readiness and functionality of surgical and critical care equipment.
- Diagnostic Imaging Centers:
- Overseeing the operation and maintenance of MRI, CT scanners, and X-ray machines.
Patient Monitoring and Diagnostic Devices
- Examples:
- ECG machines, infusion pumps, dialysis machines, and anesthesia devices.
- Responsibilities:
- Ensuring continuous operation of monitoring devices in ICUs and emergency departments.
Health Information Technology Integration
- Clinical Information Systems:
- Integrating devices with EHR systems for real-time patient data access.
- Remote Monitoring Solutions:
- Managing telemedicine platforms and wearable patient monitoring systems.
Emergency and Disaster Preparedness
- Role in Crisis Management:
- Preparing contingency plans for equipment functionality during power outages, pandemics, or natural disasters.
- Critical Equipment Readiness:
- Ensuring backup systems and emergency medical devices are operational.
Applications of Clinical Engineering
Medical Imaging Systems
- Management of Diagnostic Devices:
- CT scanners, MRI machines, ultrasound systems, and X-rays.
- Responsibilities:
- Regular calibration and quality assurance checks to maintain imaging accuracy.
Life Support Systems
- Critical Equipment:
- Ventilators, defibrillators, anesthesia machines, and dialysis units.
- Responsibilities:
- Ensuring consistent operation, especially in intensive care and emergency units.
Surgical Equipment
- Operating Room Devices:
- Surgical robots, electrosurgical units, and sterilization systems.
- Responsibilities:
- Managing technology to ensure precision and safety during surgeries.
Patient Monitoring Systems
- Devices Managed:
- ECG monitors, pulse oximeters, blood pressure monitors.
- Responsibilities:
- Continuous monitoring and maintenance to ensure uninterrupted patient care.
Laboratory and Diagnostic Equipment
- Examples:
- Blood analyzers, PCR machines, and diagnostic kits.
- Responsibilities:
- Routine performance checks for accurate diagnostic results.
Emerging Technologies in Clinical Engineering
Artificial Intelligence (AI) and Machine Learning
- Applications:
- Predictive maintenance of medical devices.
- AI-driven diagnostics integrated into imaging systems.
Internet of Medical Things (IoMT)
- Applications:
- Networked devices for remote patient monitoring.
- Real-time tracking of equipment status.
Robotics and Automation
- Applications:
- Robotic-assisted surgery and automated drug dispensers.
- Automation in sterilization and inventory management.
3D Printing in Medical Devices
- Applications:
- Custom implants, surgical guides, and prosthetics.
- On-demand manufacturing of medical tools.
Cybersecurity in Medical Devices
- Importance:
- Protecting patient data and device integrity from cyber threats.
- Applications:
- Implementing security protocols for networked medical devices.
Challenges in Clinical Engineering
Regulatory Compliance:
- Navigating complex and evolving regulatory frameworks.
- Ensuring devices meet FDA, ISO, and CE certification requirements.
Technology Integration:
- Integrating diverse devices with hospital IT systems.
Budget Constraints:
- Balancing high-quality equipment acquisition with budget limitations.
Rapid Technological Advancements:
- Keeping pace with emerging medical technologies.
Data Security:
- Safeguarding medical device networks against cybersecurity risks.
Future Trends in Clinical Engineering
Smart Hospitals:
- Integration of IoT devices for intelligent, automated healthcare delivery.
Telemedicine Expansion:
- Remote monitoring and diagnostics for patient care continuity.
Predictive Maintenance with AI:
- AI-driven analytics to anticipate device failures and reduce downtime.
Sustainable Healthcare Technology:
- Eco-friendly designs and green disposal practices for medical devices.
Advanced Robotics and Automation:
- Greater reliance on robotics for surgical procedures and patient care.
Why Study Clinical Engineering
Managing Medical Technology in Healthcare Settings
Clinical engineering focuses on the safe and effective use of medical technology in hospitals. Students learn how to manage, maintain, and evaluate medical devices. This ensures that healthcare facilities operate efficiently and safely.
Device Regulation and Compliance
Students are introduced to regulations, standards, and safety protocols for medical equipment. They ensure devices meet legal and clinical requirements. This knowledge is crucial for protecting patients and healthcare workers.
Support for Clinical Staff and Training
Clinical engineers work with doctors and nurses to ensure devices are used correctly. Students learn to provide training, troubleshoot problems, and enhance workflow. This fosters collaboration and improves patient care.
Innovation and Healthcare Delivery
Students explore how technology improves diagnostics, treatment, and hospital operations. They help integrate new systems and optimize healthcare delivery. This positions them as key players in modern medical environments.
Career Opportunities in Health Systems
Clinical engineers are in demand in hospitals, regulatory agencies, and device companies. Students can pursue leadership roles in technology management and policy. The field offers a meaningful career that directly impacts public health.
Clinical Engineering: Conclusion
Clinical Engineering is a cornerstone of modern healthcare, ensuring the safe, efficient, and effective use of medical devices and systems. From managing critical life-support machines to integrating advanced technologies like AI and IoT, clinical engineers play a vital role in improving patient care and healthcare operations. As medical technology continues to evolve, clinical engineering will remain essential in driving innovation, enhancing patient safety, and supporting the delivery of high-quality healthcare.
Frequently Asked Questions on Clinical Engineering
Do clinical engineers work directly with patients?
Clinical engineers rarely provide hands-on patient care, but their work has a direct impact on patient safety and outcomes. They work behind the scenes to ensure that monitors, ventilators, imaging systems, infusion pumps and other devices are safe, reliable and available when clinicians need them.
How is a clinical engineer different from a biomedical equipment technician?
Biomedical equipment technicians focus mainly on day-to-day maintenance and repair of medical devices, while clinical engineers typically take on broader responsibilities such as equipment planning, technology assessment, integration with IT systems, risk management and policy development. In practice, the two roles work closely together as part of the same technology team.
What does a typical day look like for a clinical engineer in a hospital?
A typical day may involve meeting clinicians to discuss new equipment needs, reviewing technical specifications from vendors, checking incident reports from devices, analysing maintenance data, visiting clinical areas to assess equipment performance, and working with IT or facilities staff on integration and safety issues. Priorities can change quickly when urgent equipment problems arise.
Which subjects should pre-university students focus on if they are interested in clinical engineering?
Students can focus on physics, mathematics and basic electronics, alongside biology or human physiology. At university, degrees in biomedical engineering, electrical or electronic engineering with healthcare modules, or related programmes provide a good pathway. Interest in hospitals, patient care and practical problem-solving is just as important as technical knowledge.
Is clinical engineering mainly technical, or does it involve management and communication as well?
Clinical engineering is both technical and managerial. Clinical engineers need to understand devices, standards and networks, but they also manage budgets, write reports and policies, negotiate with vendors and explain technical issues to clinical staff. Strong communication and the ability to translate between engineering and clinical perspectives are vital.
What kinds of career paths are available in clinical engineering?
Graduates can work as clinical engineers in hospitals, health systems, or ministries of health, and may later move into leadership roles such as head of clinical engineering, technology manager or quality and safety specialist. Some work for regulatory agencies, consulting firms or medical device companies, focusing on device safety, usability and hospital integration.
How is the role of clinical engineers changing with digital health and connected devices?
As more devices are connected to hospital networks and electronic health records, clinical engineers are increasingly involved in cybersecurity, interoperability projects and data-driven decision-making. They collaborate closely with IT departments and informatics teams to ensure that complex technology ecosystems support safe and efficient patient care.
Clinical Engineering: Review Questions and Answers
These review questions focus on the core ideas of clinical engineering, including the life-cycle management of medical devices, patient safety, technology assessment, informatics, regulation, and future trends in technology-enabled healthcare.-
What is clinical engineering, and how does it relate to biomedical engineering?
Answer: Clinical engineering is a specialised area within biomedical engineering that focuses on the application and management of medical technologies in real healthcare settings. While biomedical engineering covers the design and development of medical devices and systems, clinical engineering ensures that these technologies are safely selected, implemented, maintained and integrated into everyday patient care in hospitals and clinics. -
What are the main stages of the medical equipment life cycle that clinical engineers manage?
Answer: Clinical engineers are involved in planning and needs assessment, technology evaluation and procurement, installation and acceptance testing, routine maintenance and performance verification, incident investigation and corrective action, and finally decommissioning and replacement. Managing this full life cycle helps healthcare organisations use equipment safely, efficiently and cost-effectively over many years. -
How do clinical engineers contribute to patient safety in hospitals?
Answer: Clinical engineers contribute to patient safety by ensuring that medical devices are correctly installed, regularly inspected and properly maintained. They develop preventive maintenance schedules, perform safety and performance checks, verify alarms and backup systems, and support staff training on correct device use. They also analyse equipment-related incidents, identify root causes and recommend corrective actions to prevent recurrence. -
In what ways do clinical engineers support the procurement and evaluation of new medical equipment?
Answer: Clinical engineers evaluate clinical requirements with healthcare staff, review technical specifications and performance data from vendors, and assess how new equipment will integrate with existing infrastructure, including power, gases and IT networks. They help compare options in terms of safety, usability, interoperability and total cost of ownership, providing objective recommendations that support evidence-based procurement decisions. -
How does clinical engineering intersect with healthcare informatics and connected medical devices?
Answer: As more devices are networked and send data directly to electronic health record systems, clinical engineers work with healthcare informatics and IT teams to ensure interoperability, data integrity and cybersecurity. They help configure device interfaces, manage network connectivity, and establish procedures for monitoring and updating connected equipment so that clinical data flows reliably and securely into clinical information systems. -
What role do clinical engineers play in regulatory compliance and adherence to standards?
Answer: Clinical engineers help organisations comply with local and international regulations and standards related to medical devices, electrical safety, risk management and quality systems. They keep up to date with regulatory requirements, ensure that devices are labelled, tested and documented correctly, and participate in audits and inspections. Their work supports accreditation, reduces legal and safety risks, and promotes a culture of safe technology use. -
How do clinical engineers approach risk management for medical technologies?
Answer: Clinical engineers use risk management frameworks to identify potential hazards associated with devices, estimate the likelihood and consequences of failures, and implement control measures such as maintenance strategies, alarms, backup systems and user training. They review incident reports and near misses to refine risk assessments and adjust policies, creating a continuous loop of monitoring, learning and improvement. -
In what ways can clinical engineering support cost management in healthcare facilities?
Answer: Clinical engineers contribute to cost management by optimising the use and maintenance of equipment. They design preventive maintenance programmes that extend device lifetimes, analyse utilisation data to identify underused or duplicated equipment, and advise on repair versus replacement decisions. They also help negotiate service contracts and warranties and evaluate whether new technologies are likely to deliver sufficient clinical and operational benefits to justify their cost. -
Why is training and education of clinical staff important from a clinical engineering perspective?
Answer: Even well-designed devices can cause harm if used incorrectly. Clinical engineers develop and deliver training sessions, quick guides and competency checks so that staff understand how to operate equipment safely, respond to alarms and recognise signs of malfunction. Effective training reduces user errors, supports consistent use of safety features and helps clinicians feel confident when working with complex technologies in demanding clinical environments. -
What emerging trends are reshaping the role of clinical engineers in modern healthcare systems?
Answer: Emerging trends include the growth of connected and wearable devices, telemedicine platforms, integrated operating theatres and intensive care units, and the use of data analytics and artificial intelligence in equipment management and clinical decision support. Clinical engineers are increasingly involved in cybersecurity for medical devices, strategic technology planning, and projects that link engineering, informatics and clinical teams to create safer, more coordinated technology-enabled care.
Clinical Engineering: Thought-Provoking Questions
1. How does clinical engineering bridge the gap between medical technology and patient care?
Answer: Clinical engineering acts as a bridge by ensuring that medical devices used in patient care are reliable, effective, and safe. Clinical engineers integrate cutting-edge technologies with healthcare practices by selecting the right equipment, performing routine maintenance, and training staff to use devices correctly. This ensures that devices, such as ventilators or imaging machines, operate optimally, minimizing risks and enhancing patient outcomes.
2. Why is preventive maintenance critical for medical devices, and how does it impact healthcare delivery?
Answer: Preventive maintenance is essential for ensuring the functionality, safety, and reliability of medical devices. Regular checks and servicing minimize the risk of unexpected failures, which can be life-threatening during critical procedures. By reducing downtime, preventive maintenance enhances the efficiency of healthcare delivery, saves costs on emergency repairs, and ensures consistent patient care.
3. How can clinical engineers balance innovation with cost-effectiveness in medical technology procurement?
Answer: Clinical engineers evaluate both the performance and cost of medical devices during procurement. They consider factors such as long-term maintenance costs, compatibility with existing systems, and the device’s impact on patient care. By conducting cost-benefit analyses, engineers ensure that investments in new technologies are justifiable and aligned with the institution’s financial and clinical goals.
4. In what ways can clinical engineers address cybersecurity threats in networked medical devices?
Answer: Clinical engineers tackle cybersecurity threats by implementing robust security measures such as firewalls, encryption, and regular software updates. They also work closely with IT departments to monitor networks, identify vulnerabilities, and develop contingency plans for potential breaches. Protecting patient data and ensuring device reliability in the face of cyberattacks are critical components of their role.
5. How do clinical engineers ensure compliance with regulatory standards, and why is this important?
Answer: Clinical engineers ensure compliance by staying updated on standards set by regulatory bodies like the FDA or ISO. They conduct regular audits, maintain documentation, and follow safety protocols for medical devices. Compliance is vital to prevent legal liabilities, protect patient safety, and uphold the institution’s accreditation and reputation.
6. What are the ethical considerations involved in clinical engineering, particularly in resource-limited settings?
Answer: In resource-limited settings, clinical engineers face ethical dilemmas regarding the allocation of scarce medical devices. They must prioritize patient safety and equity while making decisions about equipment use and procurement. Ethical considerations also include transparency in device performance and ensuring that all patients, regardless of socioeconomic status, have access to safe and effective technologies.
7. How can data from medical devices be leveraged to improve healthcare outcomes, and what challenges might arise?
Answer: Data from devices like monitors or imaging machines can be analyzed to track patient trends, predict complications, and personalize treatment plans. However, challenges include ensuring data accuracy, managing large datasets, and addressing privacy concerns. Clinical engineers must collaborate with healthcare informatics teams to overcome these issues and maximize the utility of device-generated data.
8. How can artificial intelligence (AI) enhance the role of clinical engineering in healthcare?
Answer: AI can automate routine tasks such as device diagnostics and maintenance scheduling, freeing clinical engineers to focus on complex issues. AI algorithms can also analyze device data to identify patterns and predict failures before they occur, improving preventive maintenance. Furthermore, AI-powered devices can assist in diagnostics, enhancing clinical decision-making.
9. What strategies can clinical engineers use to ensure effective integration of new technologies into existing healthcare systems?
Answer: Effective integration involves conducting compatibility tests, training healthcare staff, and gradually phasing in new technologies while maintaining old systems as backups. Clinical engineers must also coordinate with stakeholders to ensure smooth transitions and address concerns related to workflows and data integration.
10. How does the Internet of Medical Things (IoMT) revolutionize clinical engineering, and what are the potential risks?
Answer: IoMT connects medical devices to a network, enabling real-time monitoring and remote management. This revolutionizes healthcare by improving device efficiency and enabling telemedicine. However, risks include increased vulnerability to cyberattacks and data breaches, which clinical engineers must mitigate through robust security measures and regular updates.
11. In what ways can clinical engineers contribute to disaster preparedness and emergency response in healthcare facilities?
Answer: Clinical engineers play a vital role in disaster preparedness by ensuring that critical medical devices are functional and readily available. They develop emergency plans for equipment deployment, maintain backup power systems, and train staff on operating devices under adverse conditions. Their expertise ensures continuity of care during emergencies.
12. How can clinical engineers drive sustainability in healthcare technology management?
Answer: Clinical engineers can promote sustainability by implementing green practices, such as recycling old equipment, reducing energy consumption in devices, and extending the lifespan of medical technologies through proper maintenance. They can also prioritize the procurement of eco-friendly devices and advocate for sustainable healthcare policies.
These questions and answers encourage students to explore clinical engineering’s multifaceted role, fostering curiosity and critical thinking while highlighting its impact on modern healthcare systems.
