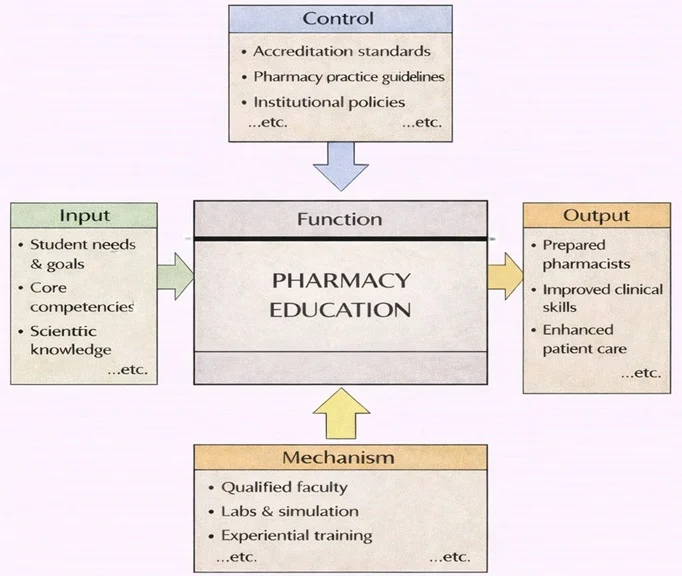
Pharmacy Education can be understood as a structured transformation process. On the left, it begins with key inputs such as student needs and goals, required core competencies, and foundational scientific knowledge. From above, controls like accreditation standards, pharmacy practice guidelines, and institutional policies shape what must be covered, how learning is assessed, and what “safe practice” looks like. From below, mechanisms—qualified faculty, laboratories and simulation resources, and experiential training sites—provide the capability to teach, coach, and evaluate learners in realistic settings. When these elements work together, the function produces clear outputs: graduates prepared for pharmacy roles, stronger clinical and decision-making skills, and ultimately better, safer patient care in real-world practice.
Pharmacy is a vital field within healthcare that focuses on the preparation, dispensing, and appropriate use of medications. It bridges the gap between medical science and patient care, ensuring that medicines are used safely and effectively. Pharmacy encompasses not only the distribution of drugs but also the science behind their development, their interactions with the body, and their role in treating and preventing diseases.
Pharmacists are highly trained healthcare professionals who collaborate with doctors, nurses, and other medical staff to optimize drug therapies for patients. Beyond dispensing medications, pharmacists educate patients about drug usage, manage potential side effects, and contribute to the development of new therapeutic solutions. Pharmacy is both a science and a practice, combining deep knowledge of chemistry, biology, information technology, and medicine with the practical skills needed for patient care. Pharmacists are also required to have good public relations and management skills, and good knowledge in psychology, and public health issues.
[This image illustrates the evolving role of pharmacists in a high-tech healthcare ecosystem. A pharmacist is shown compounding medication using a mortar and pestle, surrounded by shelves of drugs, laboratory glassware, and advanced scientific equipment. The background features digital interfaces, molecular diagrams, and a glowing DNA-embedded medical symbol—symbolizing the intersection of pharmacology, biotechnology, and data science. The scene captures how pharmacy blends chemistry, patient care, and emerging technologies to ensure safe and effective therapeutic solutions.]
Table of Contents
Focus of Pharmacy
The primary focus of pharmacy is to ensure the safe, effective, and rational use of medications. This involves understanding the complexities of drug development, the biological effects of drugs on the human body, and the social and ethical considerations of medication use. Pharmacists play a critical role in both individual patient care and broader public health initiatives.
Pharmacy is rooted in scientific research and practical application. It includes the discovery of new drugs, the formulation of medications, the monitoring of their effects, and the education of both healthcare professionals and patients. The goal is to improve health outcomes while minimizing risks and costs.
Key Areas in Pharmacy
1. Pharmacology
- Definition: The study of how drugs interact with biological systems, focusing on their effects, mechanisms of action, and therapeutic uses.
- Subfields:
- Pharmacodynamics: Examines how drugs affect the body, including their mechanisms of action.
- Pharmacokinetics: Studies how the body absorbs, distributes, metabolizes, and excretes drugs.
- Applications:
- Determining appropriate drug dosages and administration routes.
- Understanding drug interactions and side effects.
- Examples:
- Researching how antidepressants alter neurotransmitter levels.
- Studying the effects of insulin in managing diabetes.
2. Pharmaceutical Chemistry
- Definition: The science of designing and developing new drugs and optimizing their chemical formulations.
- Key Areas:
- Drug Design: Using computational models to predict how molecules will interact with biological targets.
- Formulation Science: Developing stable and effective drug delivery systems, such as tablets, injections, and inhalers.
- Applications:
- Creating life-saving medications, such as antiviral drugs for HIV.
- Innovating sustained-release formulations to improve patient compliance.
3. Clinical Pharmacy
- Definition: A patient-centered branch of pharmacy that focuses on optimizing drug therapies and improving health outcomes.
- Role of Clinical Pharmacists:
- Advising healthcare teams on selecting and managing medications.
- Monitoring patients for adverse drug reactions and interactions.
- Applications:
- Individualizing drug therapies for cancer patients based on genetic profiles.
- Educating patients on managing chronic conditions like hypertension.
4. Community and Hospital Pharmacy
- Community Pharmacy:
- Focuses on providing medications and health advice directly to the public.
- Examples: Dispensing prescriptions, offering vaccinations, and counseling on over-the-counter medications.
- Hospital Pharmacy:
- Involves managing and dispensing medications in hospital settings.
- Examples: Preparing intravenous drugs and collaborating with medical teams on treatment plans.
Applications of Pharmacy
1. Ensuring Safe and Effective Use of Medications
- Pharmacists play a crucial role in preventing medication errors and ensuring that drugs are used appropriately.
- Examples:
- Counseling patients on correct dosages and potential side effects.
- Reviewing prescriptions to prevent harmful drug interactions.
2. Researching New Treatments for Diseases
- Pharmacists contribute to the development of innovative therapies for conditions such as cancer, heart disease, and rare genetic disorders.
- Examples:
- Developing monoclonal antibodies for autoimmune diseases.
- Investigating novel antiviral drugs to combat emerging infections.
3. Public Health and Preventive Care
- Pharmacists support public health initiatives, such as vaccination campaigns and health screenings.
- Examples:
- Administering flu vaccines in community pharmacies.
- Conducting diabetes risk assessments.
4. Advancing Personalized Medicine
- With advancements in genomics, pharmacy is moving toward personalized medicine, tailoring treatments to individual genetic profiles.
- Examples:
- Prescribing targeted cancer therapies based on molecular diagnostics.
Emerging Trends in Pharmacy
Digital Health and Telepharmacy
- Remote consultations and digital tools are expanding access to pharmacy services.
- Examples: Mobile apps for medication reminders and telepharmacy platforms for virtual counseling.
Biopharmaceuticals
- The rise of biologics, such as vaccines and gene therapies, is transforming treatment options for complex diseases.
Artificial Intelligence (AI) in Drug Development
- AI is accelerating drug discovery by analyzing vast datasets to identify potential candidates for development.
Sustainable Pharmacy Practices
- Reducing pharmaceutical waste and developing eco-friendly drug manufacturing processes.
Challenges in Pharmacy
Medication Errors
- Ensuring accurate prescribing, dispensing, and administration of drugs remains a critical challenge.
Antimicrobial Resistance
- The misuse and overuse of antibiotics contribute to the growing threat of drug-resistant infections.
Access to Medications
- Ensuring equitable access to essential medications in underserved regions is a global priority.
Rapid Advancements
- Keeping up with evolving technologies and treatment paradigms requires continuous education and adaptation.
Future Directions in Pharmacy
Integration with Genomics
- Expanding the use of pharmacogenomics to create more effective and safer drug therapies.
Enhanced Patient Engagement
- Using digital tools and personalized counseling to empower patients in managing their health.
Global Collaboration
- Strengthening international partnerships to address global health challenges, such as pandemics and supply chain disruptions.
Innovations in Drug Delivery
- Developing advanced delivery systems, such as nanotechnology-based drugs and wearable drug-delivery devices.
Why Study Pharmacy
Understanding the Science of Medicines and Their Effects
Contributing to Patient Care and Public Health
Bridging Science, Healthcare, and Communication
Exploring Opportunities in Research, Innovation, and Industry
Preparing for a Respected and Dynamic Career
Pharmacy: Conclusion
Pharmacy is an indispensable field that combines scientific innovation with practical care to improve health outcomes. By focusing on pharmacology, pharmaceutical chemistry, and clinical applications, it ensures the safe and effective use of medications while driving forward advancements in treatment. With emerging technologies and evolving healthcare needs, pharmacy continues to adapt and expand, playing a central role in addressing global health challenges and enhancing patient care. The future of pharmacy lies in its ability to integrate cutting-edge science with compassionate service, ensuring that medications remain a cornerstone of modern medicine.
Frequently Asked Questions – Pharmacy
What is Pharmacy in simple terms?
Pharmacy is the health-care field that specialises in medicines — their design, preparation, dispensing, and safe use. Pharmacists ensure medications are used effectively and safely for patients, and often provide advice, counselling, and healthcare support beyond just handing out prescriptions.
What kinds of knowledge and science does pharmacy draw on?
Pharmacy draws on biomedical sciences (like anatomy, physiology, biochemistry), pharmaceutical sciences, chemistry (medicinal chemistry, pharmaceutics), pharmacology, and also aspects of public health, ethics and patient-care practices. This mix helps pharmacists understand how drugs work and how to use them safely and effectively.
What roles can pharmacists play besides dispensing medication?
Beyond dispensing, pharmacists can provide clinical services, review medications for safety and efficacy, counsel patients on drug use, manage medication therapy, advise doctors on drug interactions, support public health initiatives, and work in research, regulatory affairs, or the pharmaceutical industry.
What kinds of workplaces and career paths exist for pharmacy graduates?
Careers include community pharmacy, hospital pharmacy, clinical pharmacy, pharmaceutical industry (research and development, manufacturing), regulatory affairs, drug safety (pharmacovigilance), quality assurance, academia, research, and public health or global-health roles.
Which school subjects help prepare for studying pharmacy at university?
Strong foundations in biology, chemistry, and often mathematics are very useful because pharmacy involves drug science, human biology, and quantitative reasoning. Physics and other sciences may also help, especially for topics like pharmacology and pharmaceutics. Good communication and critical thinking skills are also important for patient counselling and professional responsibilities.
What does a typical pharmacy degree program include?
A pharmacy degree usually includes biomedical sciences (anatomy, physiology, biochemistry), pharmaceutical sciences (drug design, pharmaceutics, pharmacology), pharmacotherapy, ethics, patient-care training, and often practical placements or internships. The curriculum aims to build both scientific knowledge and professional competence.
What is pharmaceutics and how does it relate to pharmacy?
Pharmaceutics is a branch of pharmaceutical science that deals with the formulation and delivery of drugs — turning chemical substances into usable medicines, determining dosage forms (tablets, capsules, injections), and ensuring stability and effectiveness. It is foundational for designing safe and effective medications.
What is medicinal chemistry or pharmacognosy and how are they part of pharmacy?
Medicinal chemistry and pharmacognosy are disciplines within pharmacy focused on discovering, designing, and developing new drugs. They study chemical and biochemical properties of drugs, how they interact with the body, and work to optimise molecules for therapeutic use — combining chemistry, biology, and pharmacology.
Is pharmacy only about drugs and dispensing — or is patient-care part of it too?
Pharmacy today involves much more than just dispensing. Modern pharmacists often engage in direct patient care: reviewing medication regimens, counselling on safe use, checking for drug interactions, promoting public health, and helping with chronic disease management. They act as a bridge between medicine, patients, and the healthcare system.
What are some challenges and responsibilities that come with being a pharmacist?
Pharmacists must stay current with new drugs, guidelines, and research, ensure correct dosages, avoid harmful interactions, respect patient privacy, and communicate clearly. They may also face pressures related to regulation, quality control, and balancing safety with access. Their responsibility includes ensuring that medication is effective and safe for each patient.
What kinds of further specialisations are possible within pharmacy?
Pharmacists can specialise in clinical pharmacy, hospital pharmacy, research and development, regulatory affairs, pharmacovigilance (drug safety), drug formulation, quality assurance, community health pharmacy, and even academic or teaching roles. Some go into public health, global health, or pharmaceutical industry leadership roles.
How does the Pharmacy page on Prep4Uni.online support my study and career planning?
The Pharmacy page on Prep4Uni.online introduces core concepts of pharmaceutical science, explains what studying pharmacy involves, links school subjects to university requirements, outlines career paths, and provides insight into the roles, responsibilities and opportunities available to future pharmacists. This helps you explore whether pharmacy matches your interests and strengths.
Pharmacy: Review Questions and Answers:
1. What is pharmacy and why is it a critical component of healthcare?
Answer: Pharmacy is the science and practice of preparing, dispensing, and reviewing drugs, ensuring their safe and effective use to promote health. It is a critical component of healthcare because pharmacists play a vital role in advising patients, preventing medication errors, and optimizing treatment outcomes. Their expertise ensures that medications are used appropriately, improving patient safety and therapeutic efficacy. By bridging clinical care and pharmaceutical science, pharmacy contributes significantly to overall public health.
2. How do pharmacists contribute to patient safety and medication management?
Answer: Pharmacists contribute to patient safety by verifying prescriptions, counseling patients, and monitoring for potential drug interactions and adverse reactions. They use their in-depth knowledge of medications to ensure that each patient receives the correct dosage and formulation tailored to their specific needs. Through comprehensive medication management, pharmacists help to prevent errors and improve adherence to treatment plans. Their vigilance and expertise are essential in minimizing risks and promoting positive health outcomes.
3. What role does clinical research play in the field of pharmacy?
Answer: Clinical research in pharmacy is crucial as it underpins the development of new drugs, therapies, and best practices for patient care. It involves rigorous testing and evaluation of medications to ensure they are safe and effective for public use. Pharmacists engage in research to advance scientific understanding and contribute to evidence-based practice. This research not only improves current treatment protocols but also leads to innovations that can transform healthcare delivery in the future.
4. How has technology transformed modern pharmacy practice?
Answer: Technology has transformed modern pharmacy practice by introducing digital tools for prescription management, electronic health records, and automated dispensing systems. These advancements enhance the accuracy and efficiency of medication dispensing and allow pharmacists to access patient data quickly for better clinical decision-making. Moreover, technology facilitates telepharmacy services, extending expert care to remote and underserved areas. Overall, these innovations improve patient safety, streamline workflows, and enable personalized medication management.
5. What are the key challenges faced by the pharmacy profession today?
Answer: The pharmacy profession faces several challenges including the rapid pace of drug development, increasing regulatory demands, and the need to integrate advanced technologies into practice. Pharmacists must continuously update their skills to keep pace with evolving treatments and complex healthcare systems. Balancing clinical responsibilities with administrative tasks also presents ongoing challenges. Addressing these issues requires effective professional development, strategic planning, and collaborative efforts within the healthcare community.
6. How does pharmacy education prepare students for the complexities of modern healthcare?
Answer: Pharmacy education prepares students by providing a rigorous curriculum that combines theoretical knowledge with practical, hands-on experience in clinical settings. Students learn about pharmacology, medicinal chemistry, and therapeutics, which are critical for understanding how drugs work and how they are used safely. Educational programs also emphasize communication, ethics, and problem-solving skills, ensuring graduates are well-equipped to manage complex patient cases. This comprehensive training is essential for meeting the demands of modern healthcare and providing high-quality patient care.
7. What is the significance of interdisciplinary collaboration in pharmacy practice?
Answer: Interdisciplinary collaboration in pharmacy practice is significant because it allows pharmacists to work alongside physicians, nurses, and other healthcare professionals to develop comprehensive treatment plans. This collaborative approach improves patient outcomes by ensuring that all aspects of a patient’s care are considered. Pharmacists contribute their expertise in medication management while learning from other disciplines, leading to more holistic and effective healthcare solutions. The synergy created by interdisciplinary teamwork is essential for addressing complex medical conditions and advancing patient safety.
8. How do regulatory frameworks impact the practice of pharmacy?
Answer: Regulatory frameworks impact the practice of pharmacy by establishing standards for drug safety, efficacy, and ethical conduct. These regulations ensure that all medications dispensed to patients meet stringent quality criteria and that pharmacists adhere to best practices. Compliance with these regulations is essential for protecting public health and maintaining trust in the healthcare system. While regulatory requirements can be complex and demanding, they provide a necessary structure that guides safe and effective pharmacy practice.
9. What are the benefits of continuing education for pharmacy professionals?
Answer: Continuing education is beneficial for pharmacy professionals as it ensures they remain current with the latest developments in drug therapies, technological advancements, and regulatory changes. Ongoing professional development enhances their clinical skills, supports evidence-based practice, and improves patient care. It also fosters lifelong learning and adaptability, which are essential in a rapidly evolving healthcare environment. By participating in continuing education, pharmacists can maintain their competency, expand their knowledge, and contribute to the advancement of the pharmacy field.
10. How can pharmacists contribute to public health initiatives through their practice?
Answer: Pharmacists contribute to public health initiatives by engaging in preventive care, such as immunization programs, health screenings, and patient education on chronic disease management. They serve as accessible healthcare providers who offer advice on medication use, lifestyle changes, and disease prevention strategies. Their unique position in the community enables them to monitor public health trends and advocate for policies that improve health outcomes. Through these efforts, pharmacists play a crucial role in enhancing the overall well-being of the populations they serve.
Pharmacy: Thought-Provoking Questions and Answers:
1. How might emerging technologies such as machine learning and predictive analytics transform pharmacy practice in the near future?
Answer:
Emerging technologies like machine learning and predictive analytics are set to revolutionize pharmacy practice by enhancing the precision and efficiency of medication management. Machine learning algorithms can analyze large datasets from electronic health records, genetic information, and clinical trials to predict patient responses to various medications, thus optimizing treatment plans. Predictive analytics can forecast potential drug interactions and adverse effects, enabling pharmacists to intervene before issues arise. This integration of advanced technology not only improves patient outcomes but also streamlines the workflow in pharmacies, reducing errors and enhancing the overall quality of care.
Additionally, these technologies can support personalized medicine by tailoring drug therapies to individual patient profiles, leading to more targeted and effective treatments. They can also assist in inventory management and supply chain optimization, ensuring that the right medications are available at the right time. As these innovations continue to develop, they will likely become integral to the daily operations of pharmacy practice, driving a significant transformation in healthcare delivery.
2. In what ways can telepharmacy expand access to quality healthcare, particularly in underserved regions?
Answer:
Telepharmacy has the potential to greatly expand access to quality healthcare by leveraging digital communication technologies to provide remote pharmaceutical services. In underserved regions where access to pharmacists may be limited, telepharmacy enables patients to consult with healthcare professionals via video conferencing, secure messaging, and mobile apps. This approach ensures that individuals receive timely advice on medication use, dosage adjustments, and potential side effects, regardless of their geographic location. Telepharmacy also allows for remote prescription verification and monitoring, which can improve the accuracy and safety of medication dispensing.
Moreover, telepharmacy can support rural healthcare initiatives by reducing the need for patients to travel long distances to access pharmacy services. It promotes continuity of care by facilitating regular follow-ups and real-time monitoring of patients with chronic conditions. By bridging the gap between urban and rural healthcare facilities, telepharmacy not only improves patient outcomes but also contributes to a more equitable healthcare system. The integration of telepharmacy into healthcare networks is poised to transform the delivery of pharmaceutical care and enhance overall public health.
3. How can personalized medicine influence the future role of pharmacists in patient care?
Answer:
Personalized medicine is reshaping the future role of pharmacists by shifting the focus from generalized drug dispensing to customized therapeutic strategies tailored to individual patient needs. As genomic data and advanced diagnostics become more integrated into clinical practice, pharmacists will increasingly be involved in interpreting genetic information to select the most appropriate medications and dosages. This personalized approach ensures that treatments are not only effective but also minimize adverse effects, leading to improved patient outcomes. Pharmacists will need to develop expertise in genomics and bioinformatics to effectively contribute to personalized medicine initiatives, further expanding their role in healthcare.
Furthermore, the evolution of personalized medicine will likely lead to greater collaboration between pharmacists and other healthcare professionals. By working closely with physicians, genetic counselors, and researchers, pharmacists can help design and implement individualized care plans that reflect the unique health profiles of their patients. This collaborative model enhances the overall quality of care and reinforces the pharmacist’s position as an essential member of the healthcare team, dedicated to delivering optimized and patient-centered treatment solutions.
4. What ethical challenges might arise from the increasing use of digital data in pharmacy, and how can these be mitigated?
Answer:
The increasing use of digital data in pharmacy raises several ethical challenges, particularly concerning patient privacy, data security, and informed consent. As pharmacies collect and analyze vast amounts of sensitive patient information, there is a heightened risk of data breaches and unauthorized access, which can compromise patient confidentiality. Additionally, the use of predictive analytics and AI in medication management raises questions about the transparency of decision-making processes and the potential for algorithmic bias. Ensuring that patients are fully informed about how their data is used and securing robust data protection measures are essential steps to mitigate these ethical concerns.
To address these challenges, pharmacies must adhere to strict regulatory standards such as HIPAA and GDPR, which provide guidelines for data privacy and security. Implementing advanced encryption techniques, regular security audits, and transparent data management policies can help protect patient information. Furthermore, fostering an ethical culture that prioritizes patient consent and data integrity is crucial. By proactively addressing these issues, the pharmacy profession can build trust with patients and ensure that the benefits of digital data are realized without compromising ethical standards.
5. How might advances in pharmacogenomics influence drug therapy and patient outcomes?
Answer:
Advances in pharmacogenomics have the potential to significantly influence drug therapy by enabling healthcare providers to tailor treatments based on an individual’s genetic makeup. By analyzing genetic variations, pharmacogenomics helps predict how patients will respond to specific medications, allowing for the selection of drugs that are more effective and less likely to cause adverse reactions. This personalized approach can lead to more precise dosing, improved treatment efficacy, and overall better patient outcomes. As a result, the integration of pharmacogenomics into clinical practice represents a major step toward personalized medicine, where therapies are customized to achieve optimal results for each patient.
Moreover, the use of pharmacogenomic data can reduce healthcare costs by minimizing the trial-and-error process in drug selection, thereby decreasing the incidence of adverse drug reactions and hospitalizations. It also supports the development of targeted pharmaceuticals that address the specific needs of patient subgroups, contributing to a more efficient and effective healthcare system. As research in this field continues to advance, pharmacogenomics will play an increasingly important role in transforming patient care and shaping the future of drug therapy.
6. How can interdisciplinary collaboration improve the integration of new technologies in pharmacy practice?
Answer:
Interdisciplinary collaboration can significantly improve the integration of new technologies in pharmacy practice by bringing together experts from various fields such as computer science, engineering, and healthcare. This collaborative approach fosters innovation by combining different perspectives and expertise to develop digital solutions that are both practical and effective. For instance, partnerships between pharmacists, data scientists, and IT professionals can lead to the creation of advanced prescription management systems and personalized medicine platforms that enhance patient care and operational efficiency. Such collaborations facilitate the development and refinement of technologies that are tailored to the unique needs of the pharmacy setting.
Moreover, interdisciplinary teams can accelerate the adoption of new technologies by conducting rigorous testing and providing comprehensive training for healthcare professionals. This ensures that digital tools are seamlessly integrated into daily practice and that potential challenges are promptly addressed. By leveraging collective expertise, interdisciplinary collaboration not only enhances the technological capabilities of pharmacy practice but also drives continuous improvement and innovation in healthcare delivery.
7. How might patient engagement strategies evolve with the increasing use of mobile health applications in pharmacy?
Answer:
Patient engagement strategies are likely to evolve significantly with the increasing use of mobile health applications in pharmacy, as these technologies offer new avenues for interaction and personalized care. Mobile health applications provide patients with easy access to information about their medications, appointment reminders, and real-time health monitoring, which can enhance their involvement in their own care. These applications also facilitate direct communication between patients and pharmacists, enabling timely interventions and more personalized treatment adjustments. As a result, mobile health apps can lead to higher levels of patient satisfaction and better adherence to prescribed therapies.
In addition, the integration of mobile technology allows for the collection of patient feedback and health data, which can be used to continuously refine engagement strategies. This real-time data empowers pharmacists to develop targeted educational content and proactive care plans that address individual patient needs. As mobile health applications become more sophisticated, they will play an increasingly vital role in fostering a collaborative and responsive healthcare environment, ultimately improving overall patient outcomes.
8. What role does continuing education play in maintaining high standards in pharmacy practice?
Answer:
Continuing education plays a critical role in maintaining high standards in pharmacy practice by ensuring that pharmacists remain updated on the latest advancements in drug therapies, technologies, and regulatory requirements. Through ongoing professional development, pharmacists acquire new skills and knowledge that enhance their ability to provide safe, effective, and evidence-based care. This commitment to lifelong learning enables them to adapt to changes in the healthcare landscape and implement innovative practices in patient care. Additionally, continuing education fosters a culture of excellence and accountability within the profession, ensuring that pharmacists can meet evolving patient needs and contribute to improved health outcomes.
Furthermore, continuous education promotes interdisciplinary collaboration and the sharing of best practices among healthcare professionals. It allows pharmacists to stay informed about global trends and emerging research, which in turn drives the evolution of pharmacy practice. By investing in professional development, the pharmacy community not only enhances its clinical competencies but also strengthens the overall quality and reliability of healthcare services.
9. How might the integration of digital tools in pharmacy education change the future of the profession?
Answer:
The integration of digital tools in pharmacy education is set to transform the future of the profession by enhancing learning experiences and preparing graduates for modern healthcare challenges. Digital tools such as virtual simulations, online learning platforms, and interactive modules provide students with hands-on training and real-time feedback, which significantly improve their understanding of complex pharmaceutical concepts. These innovations facilitate a more engaging and flexible educational environment, enabling students to learn at their own pace and access a wealth of resources that were previously unavailable. As a result, future pharmacists will be better equipped with the skills needed to excel in a rapidly evolving digital healthcare landscape.
In addition, digital integration encourages interdisciplinary learning and collaboration, as students can connect with peers and experts from around the world. This exposure to diverse perspectives enriches their educational experience and fosters a more innovative and adaptive mindset. Ultimately, the adoption of digital tools in pharmacy education will not only enhance the quality of instruction but also drive the evolution of the pharmacy profession, ensuring that it remains responsive to the needs of modern patient care.
10. How can regulatory changes impact the future landscape of pharmacy practice and patient care?
Answer:
Regulatory changes have a profound impact on the future landscape of pharmacy practice and patient care by setting the standards for drug safety, quality, and ethical practice. As regulations evolve to address emerging challenges such as the integration of digital health technologies and personalized medicine, pharmacists must adapt their practices to remain compliant and provide high-quality care. These changes can lead to improvements in patient safety, better medication management, and increased accountability within the healthcare system. Moreover, proactive regulatory updates encourage innovation and drive the adoption of advanced practices, ultimately benefiting both practitioners and patients by ensuring that care is both current and effective.
In addition, regulatory reforms often result in increased collaboration between government agencies, healthcare providers, and industry stakeholders. This collaborative approach helps to streamline processes, reduce administrative burdens, and promote a more efficient healthcare system overall. As a result, the evolving regulatory landscape plays a crucial role in shaping the future of pharmacy practice, driving continuous improvement and fostering an environment where patient care is consistently enhanced.
11. How might global health trends influence pharmacy education and practice in the coming years?
Answer:
Global health trends, such as the rise in chronic diseases, aging populations, and the emergence of new pathogens, are poised to significantly influence pharmacy education and practice. These trends necessitate a shift in both the curriculum and clinical practices to address the evolving healthcare needs of diverse populations. Pharmacy education will increasingly emphasize topics such as preventive care, personalized medicine, and the use of digital health technologies to manage complex health conditions. As a result, future pharmacists will be better prepared to deliver patient-centered care that is responsive to global health challenges.
Furthermore, global health trends drive interdisciplinary collaboration and innovation, encouraging pharmacy programs to integrate insights from epidemiology, public health, and technology. This holistic approach ensures that graduates are equipped with the knowledge and skills needed to tackle modern healthcare challenges and contribute to international efforts to improve public health. Ultimately, the influence of global health trends will lead to a more dynamic, adaptable, and globally informed pharmacy practice that enhances patient outcomes and advances the field.
12. How can interdisciplinary research and collaboration enhance advancements in pharmacy practice?
Answer:
Interdisciplinary research and collaboration have the potential to greatly enhance advancements in pharmacy practice by merging expertise from diverse fields such as chemistry, biology, engineering, and data science. This collaborative approach fosters innovative solutions to complex healthcare challenges, leading to the development of new drugs, improved delivery systems, and more effective treatment protocols. By working together, experts can share insights and methodologies that accelerate the pace of discovery and streamline the translation of research findings into clinical applications, ultimately benefiting patient care.
Moreover, interdisciplinary collaboration promotes a more comprehensive understanding of the intricate interactions between drugs and the human body. It enables the integration of cutting-edge technologies such as AI and machine learning into pharmaceutical research, which can improve diagnostic accuracy and optimize treatment strategies. As a result, the synergistic effects of interdisciplinary research not only drive innovation but also lead to more robust and effective healthcare solutions, transforming the future of pharmacy practice.
