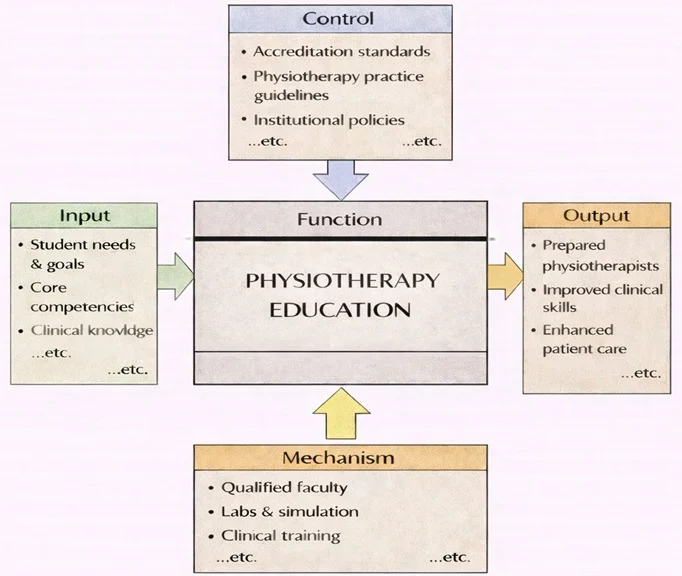
Physiotherapy Education can be understood as a structured “transformation” process. From the left, it begins with student needs and goals, along with the core competencies and clinical knowledge that the profession expects new practitioners to master. From the top, the process is guided by accreditation requirements, physiotherapy practice guidelines, and institutional policies, which define what must be covered, how learning should be assessed, and what safe practice looks like.
From the bottom, the function is enabled by the mechanisms that make training possible—qualified faculty, labs and simulation facilities, and clinical training placements where students learn in real healthcare settings. When these inputs, controls, and mechanisms work together, the output is a pipeline of prepared physiotherapists with strong clinical skills and the capacity to deliver better patient care, supporting healthier individuals and communities.
Physiotherapy, also known as physical therapy, is a healthcare profession dedicated to restoring, maintaining, and improving physical function and mobility in individuals of all ages. It employs a range of therapeutic exercises, manual techniques, and advanced technologies to alleviate pain, promote healing, and enhance overall well-being. Physiotherapists work closely with patients to develop personalized treatment plans that address specific needs, whether recovering from surgery, managing chronic conditions, or improving physical performance.
Physiotherapy plays a critical role in healthcare systems worldwide, bridging the gap between acute medical care and long-term recovery. Its applications extend beyond rehabilitation, encompassing preventive care, health education, and performance optimization. As lifestyles become more sedentary and chronic conditions more prevalent, the importance of physiotherapy in promoting active and independent living continues to grow.

This bright illustration shows a rehabilitation clinic where physiotherapists work with several patients at once. In the foreground, a therapist supports a person practicing walking with a cane, emphasizing balance training and functional mobility. Nearby, patients do guided exercises with therapy balls, resistance equipment, and light weights, while others receive hands-on treatment on therapy tables. The background displays muscle and skeleton diagrams, reinforcing the role of anatomy and biomechanics in treatment planning. The overall scene highlights physiotherapy as practical, goal-focused care that combines assessment, exercise, manual techniques, and patient coaching to improve everyday movement and quality of life.
Focus of Physiotherapy
The focus of physiotherapy is to restore and enhance physical mobility, reduce pain, and improve the quality of life for individuals affected by injuries, illnesses, or disabilities. It aims to empower patients by teaching them how to manage their conditions through exercises, lifestyle modifications, and preventive measures. Physiotherapists use evidence-based practices to ensure effective and safe treatments tailored to the unique needs of each patient.
Physiotherapy emphasizes a holistic approach, addressing not only the physical aspects of health but also the psychological and social factors that influence recovery. By fostering independence and promoting self-care, physiotherapy enhances overall well-being and reduces reliance on long-term medical interventions.
Key Areas in Physiotherapy
1. Orthopedic Physiotherapy
- Definition:
Focuses on the assessment and treatment of musculoskeletal injuries and conditions affecting bones, joints, muscles, and ligaments. - Key Conditions Treated:
- Fractures, sprains, and dislocations.
- Post-surgical rehabilitation (e.g., after joint replacements).
- Chronic conditions like arthritis and tendinitis.
- Therapeutic Techniques:
- Strengthening and stretching exercises.
- Manual therapy for joint mobilization.
- Posture correction and gait training.
- Examples:
- Assisting athletes in recovering from ACL injuries.
- Designing exercise programs for patients with lower back pain.
2. Neurological Physiotherapy
- Definition:
Specializes in managing conditions that affect the nervous system, such as strokes, Parkinson’s disease, and multiple sclerosis. - Key Goals:
- Restoring motor function and coordination.
- Reducing muscle spasticity and improving balance.
- Enhancing independence in daily activities.
- Therapeutic Techniques:
- Balance and coordination exercises.
- Electrical stimulation to activate muscles.
- Functional movement training.
- Examples:
- Helping stroke survivors regain mobility and strength.
- Teaching Parkinson’s patients exercises to improve gait and reduce tremors.
3. Pediatric Physiotherapy
- Definition:
Focuses on children with developmental, neurological, or musculoskeletal conditions. - Key Conditions Treated:
- Cerebral palsy, muscular dystrophy, and spina bifida.
- Developmental delays in motor skills.
- Congenital deformities like clubfoot.
- Therapeutic Techniques:
- Play-based therapy to engage children in movement.
- Strengthening and flexibility exercises tailored to developmental needs.
- Parental education and guidance.
- Examples:
- Helping children with cerebral palsy improve mobility using assistive devices.
- Encouraging motor skill development in infants with delayed milestones.
Applications of Physiotherapy
1. Recovery from Surgeries and Injuries
- Overview:
Physiotherapy aids in the recovery process following surgeries, accidents, or sports-related injuries. - Examples:
- Post-operative rehabilitation for knee or hip replacements.
- Strengthening and mobilization exercises after a fracture.
- Impact:
- Speeds up recovery time and prevents complications such as stiffness or muscle atrophy.
2. Managing Chronic Conditions
- Overview:
Physiotherapy helps individuals manage long-term health conditions to maintain functionality and reduce pain. - Examples:
- Tailoring exercise programs for individuals with arthritis or osteoporosis.
- Using aquatic therapy to alleviate pain in fibromyalgia patients.
- Impact:
- Improves quality of life and reduces reliance on medication.
3. Enhancing Physical Performance
- Overview:
Physiotherapists work with athletes and active individuals to optimize physical performance and prevent injuries. - Examples:
- Developing conditioning programs for runners or swimmers.
- Analyzing movement patterns to reduce injury risks.
- Impact:
- Enhances strength, endurance, and flexibility, leading to better performance.
4. Preventive Care and Health Promotion
- Overview:
Physiotherapy emphasizes prevention by addressing risk factors for injuries and chronic diseases. - Examples:
- Educating desk workers on ergonomic setups to avoid posture-related issues.
- Conducting fall prevention programs for elderly individuals.
- Impact:
- Reduces healthcare costs and improves overall health outcomes.
Emerging Trends in Physiotherapy
Tele-Physiotherapy
- Providing virtual consultations and guided exercises for remote patients.
Integration with Technology
- Using wearable devices, AI tools, and VR systems to monitor progress and enhance therapy outcomes.
Focus on Mental Health
- Addressing the psychological impact of injuries and chronic conditions through holistic approaches.
Regenerative Therapies
- Incorporating stem cell research and regenerative medicine into rehabilitation practices.
Community-Based Programs
- Expanding physiotherapy services to underserved populations through outreach and community health initiatives.
Challenges in Physiotherapy
Access to Care
- Limited availability of physiotherapy services in rural and low-income areas.
Adherence to Treatment
- Ensuring patients follow through with prescribed exercises and therapies.
Evolving Needs
- Adapting to the growing demand for physiotherapy due to aging populations and lifestyle-related conditions.
Workforce Shortages
- Addressing the shortage of trained physiotherapists globally.
Future Directions in Physiotherapy
Personalized Therapy Plans
- Leveraging data and technology to design individualized treatment programs.
Collaborative Healthcare Models
- Integrating physiotherapy with other disciplines like occupational therapy and mental health services.
Focus on Preventive Care
- Expanding physiotherapy’s role in preventing injuries and managing risk factors.
Research and Innovation
- Advancing understanding of musculoskeletal and neurological recovery through research.
Global Health Initiatives
- Strengthening the role of physiotherapy in addressing global health challenges like aging and chronic diseases.
Why Study Physiotherapy
Understanding the Science of Movement and Rehabilitation
Helping People Recover and Improve Their Quality of Life
Combining Clinical Skills with Compassionate Care
Exploring Diverse Areas of Practice and Specialization
Preparing for a Fulfilling and In-Demand Health Career
Physiotherapy: Conclusion
Physiotherapy is a vital healthcare discipline that enhances mobility, alleviates pain, and promotes overall well-being. By addressing a wide range of conditions, from acute injuries to chronic diseases, physiotherapy empowers individuals to lead active and fulfilling lives. Its applications in recovery, prevention, and performance optimization make it indispensable in modern healthcare. As technology and research continue to advance, physiotherapy will expand its reach and impact, ensuring better health outcomes and improved quality of life for diverse populations worldwide.
Frequently Asked Questions – Physiotherapy
What is physiotherapy in simple terms?
Physiotherapy is a health profession that uses movement, exercise, manual therapy, education, and advice to help people restore, maintain, or improve their physical function and quality of life. Physiotherapists work with people who have pain, injury, disability, or long-term health conditions, as well as those who want to prevent problems and stay active.
How is physiotherapy different from general medicine or surgery?
Medicine and surgery focus on diagnosing diseases, prescribing drugs, and performing operations, while physiotherapy focuses on how people move and function in daily life. Physiotherapists use assessment, movement-based treatment, and education to reduce pain, improve mobility and strength, and support recovery before or after medical or surgical treatment.
What kinds of problems do physiotherapists treat?
Physiotherapists treat a wide range of conditions, including back and neck pain, sports injuries, joint and muscle problems, stroke and neurological conditions, heart and lung conditions, balance and mobility issues in older adults, and physical difficulties related to long-term illnesses or disability.
What is the difference between physiotherapy and occupational therapy?
Physiotherapy focuses mainly on movement, physical function, and the body’s systems that support activity, such as muscles, joints, heart, and lungs. Occupational therapy focuses more on enabling people to carry out meaningful daily activities at home, school, work, or in the community, often by adapting tasks or environments in addition to working on movement and strength.
Which school subjects are helpful if I want to study physiotherapy at university?
Biology is especially important for understanding human anatomy, physiology, and how the body responds to injury and exercise. Chemistry, physics, and mathematics can also be useful, especially for biomechanics and evidence-based practice. Subjects that build communication and writing skills help with patient interaction and professional documentation.
What personal qualities are important for future physiotherapists?
Future physiotherapists need strong communication skills, empathy, patience, and the ability to motivate people who may be in pain or discouraged. They also need good observational skills, problem-solving ability, physical stamina, and a willingness to keep learning as evidence and practice change over time.
What do students typically study in a physiotherapy degree?
Physiotherapy degrees usually include anatomy and physiology, biomechanics, neuroscience, pathology, exercise science, and rehabilitation science. Students learn assessment techniques, therapeutic exercises, manual therapy, electrotherapy, respiratory and cardiovascular physiotherapy, and how to plan and progress treatment programmes. Professional practice, ethics, and research skills are also core components.
What kind of clinical placements do physiotherapy students complete?
Physiotherapy students complete supervised placements in settings such as hospitals, outpatient clinics, rehabilitation centres, community health services, sports and orthopaedic clinics, aged-care facilities, and sometimes schools or industrial workplaces. These placements allow them to apply theory, practise clinical reasoning, and work as part of multidisciplinary teams.
What are some main areas or specialisations within physiotherapy?
Major areas of physiotherapy include musculoskeletal and sports physiotherapy, cardiorespiratory physiotherapy, neurological physiotherapy, paediatric physiotherapy, geriatric physiotherapy, women’s and men’s health, community and public health physiotherapy, and occupational or industrial rehabilitation. With experience and further study, physiotherapists can specialise in one or more of these fields.
How does physiotherapy contribute to prevention and long-term health, not just recovery?
Physiotherapy is not only for injury or illness. Physiotherapists design exercise and movement programmes to improve strength, flexibility, balance, and cardiovascular fitness, helping to prevent falls, manage chronic conditions, and reduce the risk of future injuries. They also educate people about posture, workplace ergonomics, and healthy activity habits.
What kinds of workplaces and careers are available to physiotherapy graduates?
Physiotherapy graduates can work in public and private hospitals, outpatient and specialist clinics, sports medicine and performance centres, community health services, rehabilitation and aged-care facilities, schools, and workplace or occupational health settings. Some move into research, teaching, health management, or roles with sports teams and international health organisations.
How does the Physiotherapy page on Prep4Uni.online support my study and career planning?
The Physiotherapy page on Prep4Uni.online introduces key ideas about human movement, injury, and rehabilitation, and links school subjects to university-level expectations. It helps you understand what physiotherapy study involves, what skills and qualities are important, and how physiotherapy connects to wider health, sport, and rehabilitation careers.
Physiotherapy: Review Questions and Answers:
1. What is physiotherapy and what are its primary goals?
Answer: Physiotherapy is a healthcare discipline that focuses on the evaluation, treatment, and prevention of physical impairments and disabilities through physical methods such as exercise, manual therapy, and electrotherapy. Its primary goals are to improve mobility, relieve pain, restore function, and promote overall health and wellness. Through targeted interventions, physiotherapists help patients recover from injuries, manage chronic conditions, and enhance their quality of life. Additionally, physiotherapy emphasizes patient education and active participation in the recovery process, empowering individuals to maintain long-term physical well-being.
2. How do physiotherapy treatments contribute to patient rehabilitation?
Answer: Physiotherapy treatments contribute to patient rehabilitation by employing a variety of techniques that address both acute injuries and chronic conditions. These treatments often include exercise programs, manual therapies, and the use of modalities such as heat, cold, or electrical stimulation to promote healing. By focusing on improving strength, flexibility, and balance, physiotherapy helps patients regain independence and return to their daily activities. Moreover, individualized treatment plans ensure that rehabilitation is tailored to each patient’s specific needs, optimizing recovery outcomes and preventing future injuries.
3. What are the common techniques used in physiotherapy?
Answer: Common techniques used in physiotherapy include therapeutic exercises, manual therapy, electrotherapy, and hydrotherapy, among others. Therapeutic exercises are designed to improve strength, range of motion, and endurance, while manual therapy involves hands-on techniques to mobilize joints and soft tissues. Electrotherapy utilizes electrical energy to reduce pain and stimulate muscle function, and hydrotherapy uses water-based exercises to enhance rehabilitation in a low-impact environment. These diverse techniques enable physiotherapists to create comprehensive treatment plans that address various aspects of physical impairment and promote holistic recovery.
4. How does physiotherapy help in managing chronic pain?
Answer: Physiotherapy helps manage chronic pain by using a combination of exercises, manual techniques, and patient education to alleviate discomfort and improve function. By focusing on strengthening muscles, improving flexibility, and promoting proper posture, physiotherapists work to reduce the underlying causes of chronic pain. Additionally, modalities such as heat therapy, cold therapy, and electrical stimulation can provide temporary relief from pain symptoms. Patient education is also a crucial component, as it empowers individuals to manage their condition through lifestyle modifications and self-care strategies, leading to sustained pain management and improved quality of life.
5. What role does patient education play in physiotherapy?
Answer: Patient education plays a central role in physiotherapy by equipping individuals with the knowledge and skills to manage their conditions independently. Educating patients about proper exercise techniques, injury prevention, and self-management strategies helps ensure that they can maintain their progress outside of clinical sessions. This education fosters long-term adherence to treatment plans and promotes a proactive approach to health and wellness. Furthermore, informed patients are more likely to participate actively in their recovery process, leading to better outcomes and reduced dependency on continuous professional intervention.
6. How can physiotherapy be adapted for different age groups and conditions?
Answer: Physiotherapy can be adapted for different age groups and conditions through the customization of treatment plans that consider the specific needs, abilities, and developmental stages of patients. For children, physiotherapy may incorporate playful and engaging exercises that promote motor skill development and coordination, while for older adults, the focus might be on improving balance, strength, and flexibility to prevent falls and enhance mobility. For patients with chronic conditions, treatment plans are designed to manage symptoms and improve functional capacity. This personalized approach ensures that interventions are both effective and appropriate for the individual, leading to better overall outcomes.
7. What is the importance of interdisciplinary collaboration in physiotherapy?
Answer: Interdisciplinary collaboration in physiotherapy is crucial for delivering comprehensive patient care by integrating expertise from various healthcare professionals such as physicians, occupational therapists, and nutritionists. This collaborative approach ensures that all aspects of a patient’s condition are addressed, resulting in more holistic and effective treatment plans. By working together, healthcare providers can share insights and develop strategies that optimize rehabilitation and recovery. Such teamwork not only improves patient outcomes but also enhances the efficiency of healthcare delivery by ensuring a coordinated approach to treatment.
8. How does technology influence modern physiotherapy practices?
Answer: Technology influences modern physiotherapy practices by providing advanced tools that enhance diagnosis, treatment, and patient monitoring. Digital imaging, wearable sensors, and virtual reality are among the innovations that allow physiotherapists to assess movement patterns and customize interventions more accurately. These technologies enable the collection of real-time data, which can be used to adjust treatment plans and track patient progress effectively. As a result, technology integration not only improves the precision of physiotherapy but also increases patient engagement and overall treatment efficacy.
9. What challenges do physiotherapists face in their practice, and how can they overcome them?
Answer: Physiotherapists face challenges such as managing diverse patient populations, staying updated with rapidly evolving treatment technologies, and addressing complex, chronic conditions. These challenges require continuous professional development and a commitment to lifelong learning. By engaging in regular training and collaborating with other healthcare professionals, physiotherapists can refine their skills and adopt innovative approaches to treatment. Overcoming these challenges ultimately leads to more effective patient care and improved rehabilitation outcomes.
10. How do physiotherapy interventions contribute to the prevention of injuries and promotion of long-term wellness?
Answer: Physiotherapy interventions contribute to the prevention of injuries by emphasizing proactive measures such as strength training, flexibility exercises, and proper body mechanics. These interventions help to identify and correct imbalances or weaknesses before they lead to injury. In addition, physiotherapy promotes long-term wellness by encouraging regular physical activity and educating patients on injury prevention strategies. By fostering healthy movement patterns and overall physical fitness, these interventions support sustained well-being and reduce the likelihood of future injuries.
Physiotherapy: Thought-Provoking Questions and Answers
1. How might emerging wearable technologies further enhance the effectiveness of physiotherapy treatments?
Answer:
Emerging wearable technologies have the potential to significantly enhance physiotherapy treatments by providing continuous, real-time data on patient movement, muscle activity, and physiological responses. These devices can monitor a patient’s progress both during clinical sessions and in their daily lives, offering valuable insights into the effectiveness of treatment protocols. With detailed data analytics, physiotherapists can customize and adjust interventions based on precise measurements, ensuring that treatment plans are optimized for each individual’s needs. Wearable technology also facilitates early detection of potential issues, allowing for timely interventions that can prevent injuries or complications.
Furthermore, the integration of wearable devices with mobile apps and digital health platforms creates a feedback loop between patients and therapists, enhancing engagement and adherence to prescribed exercises. This seamless connection not only improves the overall effectiveness of physiotherapy but also empowers patients to take an active role in their recovery. As these technologies continue to evolve, they are likely to become indispensable tools in modern physiotherapy, driving innovation and improving patient outcomes on a broad scale.
2. In what ways can virtual reality (VR) be integrated into physiotherapy, and what benefits might it offer to patients?
Answer:
Virtual reality (VR) can be integrated into physiotherapy by creating immersive environments that simulate real-world scenarios, allowing patients to practice movements and exercises in a controlled, engaging setting. VR technology enables physiotherapists to design customized rehabilitation programs that are both interactive and adaptable to individual needs, providing patients with a unique and motivating way to engage in their therapy. This integration can be particularly beneficial for patients recovering from injuries, as VR allows for repetitive practice of movements without the risk of further injury, thereby promoting more effective and accelerated recovery.
Additionally, VR can enhance patient engagement by making therapy sessions more enjoyable and less monotonous, which may lead to increased adherence to treatment plans. The immersive nature of VR can distract patients from pain and discomfort during exercises, improving their overall experience and willingness to participate. By incorporating VR into physiotherapy, healthcare providers can offer a more dynamic and holistic approach to rehabilitation that not only improves physical outcomes but also contributes to better mental well-being.
3. How might advancements in artificial intelligence (AI) change the landscape of physiotherapy practice?
Answer:
Advancements in artificial intelligence (AI) are poised to change the landscape of physiotherapy practice by enhancing diagnostic accuracy, treatment personalization, and outcome prediction. AI can analyze vast amounts of patient data, including movement patterns, muscle activation levels, and recovery trends, to identify subtle changes that may indicate progress or potential setbacks. This information enables physiotherapists to tailor treatment plans to each patient’s specific needs, thereby optimizing rehabilitation protocols and reducing the risk of injury.
Moreover, AI-driven predictive analytics can forecast patient outcomes based on historical data and real-time inputs, allowing therapists to adjust interventions proactively. By automating routine tasks such as data collection and analysis, AI frees up physiotherapists to focus more on direct patient care and clinical decision-making. The integration of AI into physiotherapy practice not only improves efficiency and treatment efficacy but also paves the way for a more personalized, data-driven approach to patient rehabilitation and long-term wellness.
4. In what ways can interdisciplinary collaboration improve physiotherapy outcomes?
Answer:
Interdisciplinary collaboration can significantly improve physiotherapy outcomes by combining expertise from various healthcare disciplines to create comprehensive treatment plans. When physiotherapists work closely with physicians, occupational therapists, nutritionists, and psychologists, they can address all facets of a patient’s health and recovery. This collaborative approach ensures that interventions are not only focused on physical rehabilitation but also consider nutritional support, mental health, and overall lifestyle modifications. The result is a more holistic treatment strategy that enhances patient outcomes and accelerates recovery.
Furthermore, interdisciplinary teams facilitate the sharing of knowledge and best practices, leading to innovative treatment protocols and more efficient patient care. By pooling resources and insights, healthcare professionals can develop integrated solutions that address complex medical conditions and reduce the risk of re-injury. This synergy among disciplines ultimately contributes to a higher standard of care, improved patient satisfaction, and long-term health benefits that extend beyond the individual treatment session.
5. How might telehealth services expand the reach of physiotherapy to underserved populations?
Answer:
Telehealth services can expand the reach of physiotherapy to underserved populations by providing remote access to expert care and personalized rehabilitation programs. Through video consultations, digital exercise demonstrations, and remote monitoring tools, physiotherapists can deliver effective treatment to patients who may lack access to specialized care due to geographic or economic constraints. This approach reduces the need for travel and enables continuous care, ensuring that patients receive timely interventions and support regardless of their location.
Telehealth also facilitates regular follow-ups and progress tracking, which are essential for maintaining treatment efficacy and adapting rehabilitation plans as needed. By leveraging digital communication platforms, physiotherapists can collaborate with local healthcare providers and community organizations to extend their services to remote areas. This increased accessibility not only improves health outcomes for underserved populations but also contributes to a more equitable healthcare system by bridging gaps in service delivery.
6. What challenges might physiotherapists encounter when integrating new technologies into their practice, and how can these challenges be overcome?
Answer:
Physiotherapists may encounter challenges such as high costs, a steep learning curve, and resistance from patients or staff when integrating new technologies into their practice. The adoption of advanced digital tools requires significant financial investment, ongoing maintenance, and comprehensive training to ensure effective use. Additionally, some patients may be hesitant or unfamiliar with technology, which can hinder the smooth implementation of digital interventions. Overcoming these challenges involves securing funding through grants or partnerships, providing robust professional development, and gradually introducing new technologies to allow for adaptation.
To facilitate a smoother transition, physiotherapists can pilot new technologies in a controlled setting and gather feedback to make necessary adjustments before widespread adoption. Building a supportive network among colleagues and collaborating with technology experts can also help address technical issues and foster a culture of innovation. By addressing these obstacles proactively, physiotherapists can successfully integrate modern tools into their practice, enhancing both patient care and operational efficiency.
7. How can patient feedback be used to refine physiotherapy treatment protocols?
Answer:
Patient feedback is a valuable tool for refining physiotherapy treatment protocols as it provides direct insights into the effectiveness and patient experience of the interventions. By systematically collecting feedback through surveys, interviews, and digital platforms, physiotherapists can identify what aspects of a treatment plan are working well and which areas require improvement. This real-world data allows practitioners to tailor their approaches to better meet patient needs, ultimately enhancing treatment outcomes and satisfaction.
Incorporating patient feedback also fosters a collaborative environment where patients feel valued and involved in their own care. It enables physiotherapists to adjust exercises, modify techniques, and optimize the overall rehabilitation process based on individual responses. Continuous feedback loops not only improve the quality of care but also contribute to the evolution of best practices in physiotherapy, ensuring that treatment protocols remain effective and responsive to changing patient needs.
8. What is the impact of socioeconomic factors on access to physiotherapy services, and how can these disparities be addressed?
Answer:
Socioeconomic factors have a significant impact on access to physiotherapy services, as individuals from lower-income backgrounds may face barriers such as cost, transportation, and limited availability of specialized care. These disparities can lead to delays in treatment and poorer health outcomes for vulnerable populations. Addressing these issues requires targeted policies and initiatives that aim to improve accessibility, such as subsidized services, community-based programs, and telehealth solutions that reduce geographical barriers.
By collaborating with government agencies, non-profit organizations, and healthcare providers, physiotherapists can develop programs that specifically address the needs of underserved communities. These initiatives may include mobile clinics, sliding-scale fees, and partnerships with community centers to offer affordable care. Ultimately, reducing socioeconomic disparities in physiotherapy access contributes to more equitable healthcare and better overall public health outcomes.
9. How might continuous professional development impact the quality of physiotherapy care?
Answer:
Continuous professional development (CPD) is essential for maintaining and enhancing the quality of physiotherapy care by ensuring that practitioners remain up-to-date with the latest research, techniques, and technological advancements. Through ongoing training, physiotherapists can refine their skills, adopt innovative treatment protocols, and improve their ability to manage complex patient cases. CPD also fosters a culture of lifelong learning, encouraging practitioners to engage with new ideas and best practices that enhance clinical outcomes.
Moreover, regular professional development helps physiotherapists stay informed about changes in regulatory standards and emerging health trends, enabling them to adapt their practice accordingly. This commitment to ongoing education not only improves patient care but also boosts practitioner confidence and job satisfaction. As a result, CPD plays a crucial role in driving the continuous improvement of physiotherapy services and ensuring that patients receive the highest standard of care.
10. How can interdisciplinary collaboration enhance the effectiveness of physiotherapy interventions?
Answer:
Interdisciplinary collaboration enhances the effectiveness of physiotherapy interventions by bringing together experts from diverse fields such as medicine, nutrition, psychology, and biomechanics. This collaborative approach allows for the development of comprehensive treatment plans that address all aspects of a patient’s condition, from physical rehabilitation to nutritional support and mental well-being. By sharing knowledge and insights, interdisciplinary teams can identify the most effective strategies for recovery and tailor interventions to meet the unique needs of each patient.
Such collaboration also promotes innovation in treatment methods by integrating different perspectives and techniques. For instance, working with sports scientists or occupational therapists can lead to more advanced and holistic rehabilitation protocols. Ultimately, interdisciplinary collaboration results in more robust and patient-centered care, enhancing recovery outcomes and overall quality of life.
11. How might emerging trends in personalized medicine influence physiotherapy practice?
Answer:
Emerging trends in personalized medicine are likely to have a significant influence on physiotherapy practice by enabling treatments to be tailored to the unique genetic, biochemical, and environmental profiles of individual patients. Personalized physiotherapy approaches can optimize rehabilitation protocols, ensuring that interventions are specifically designed to meet the patient’s particular needs and maximize recovery outcomes. This customization may involve the use of advanced diagnostic tools and data analytics to track progress and adjust treatment plans in real time.
As personalized medicine becomes more integrated into healthcare, physiotherapists will need to collaborate closely with other specialists to develop comprehensive, individualized care plans. This evolution in practice not only improves the effectiveness of physiotherapy but also enhances patient satisfaction by providing more precise and targeted treatments. The shift towards personalized care represents a transformative change that has the potential to significantly improve long-term health outcomes and revolutionize rehabilitation strategies.
12. How can advancements in virtual simulation technology improve physiotherapy education and patient rehabilitation?
Answer:
Advancements in virtual simulation technology can greatly improve physiotherapy education and patient rehabilitation by providing immersive, interactive environments that mimic real-life clinical scenarios. In educational settings, virtual simulations allow students to practice and refine their skills in a risk-free environment, which enhances their learning and boosts confidence before working with actual patients. These simulations can replicate a wide range of conditions and treatment scenarios, enabling learners to gain comprehensive practical experience that is difficult to achieve through traditional classroom methods.
For patient rehabilitation, virtual simulation technology offers innovative tools for customized therapy that can adapt to the patient’s progress and specific needs. By engaging patients in interactive, gamified exercises, these technologies make rehabilitation more engaging and can accelerate recovery by providing immediate feedback and motivation. Overall, virtual simulations bridge the gap between theoretical knowledge and practical application, contributing to more effective education and improved patient outcomes in physiotherapy.
