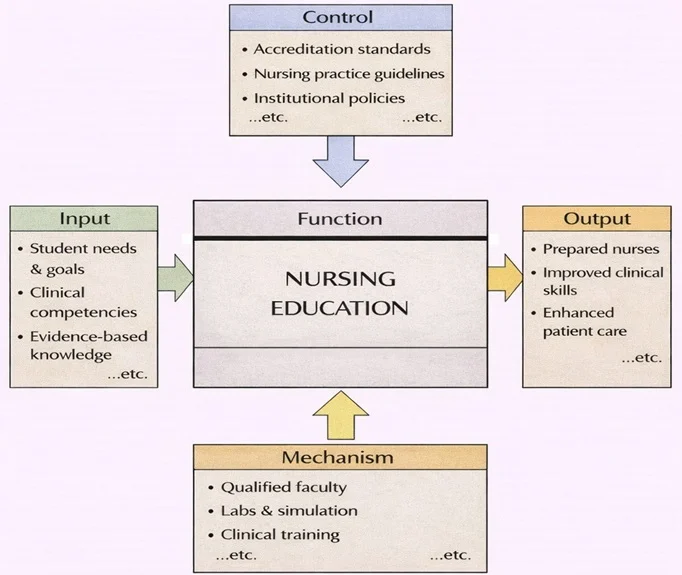
Nursing Education transforms learner needs and professional expectations into safe, capable nursing practice. As the diagram shows, the inputs include student goals, required clinical competencies, and evidence-based knowledge that nursing students must master. This work is guided by controls such as accreditation standards, nursing practice guidelines, and institutional policies, which shape what is taught, how competence is assessed, and what ethical and safety requirements must be met. The function is carried out through key mechanisms—qualified faculty, laboratories and simulation facilities, and supervised clinical training—so learning is not only theoretical but practiced and verified in realistic settings. The outputs are prepared nurses with stronger clinical skills and, ultimately, better patient care.
Nursing is a vital profession within the healthcare system, dedicated to providing compassionate care, supporting recovery, and promoting overall health. Nurses play a multifaceted role, blending clinical expertise with emotional support to address the needs of patients and their families. As frontline caregivers, they are the bridge between patients and the broader medical team, ensuring that care is not only effective but also empathetic and personalized.
The field of nursing is diverse and continually evolving, encompassing various specialties and responsibilities. It requires a balance of scientific knowledge, technical skills, and a deep commitment to ethical care. From bedside care in hospitals to health education in communities, nursing is at the core of healthcare delivery, touching lives in profound ways.

This warm, colorful image highlights nursing as both a clinical profession and a caring relationship. At the center, two nurses face each other in conversation, framed by a large heart and a heartbeat line, symbolizing empathy and patient wellbeing. Around them, nurses and healthcare staff assist patients—checking on someone in bed, offering guidance, and working in teams—showing the wide scope of nursing roles. Medical icons such as crosses and traditional healthcare symbols emphasize professionalism and safety, while the overall composition conveys the core nursing mission: attentive care, clear communication, and coordinated support for patients and families.
Table of Contents
Focus of Nursing
The primary focus of nursing is to provide holistic care that addresses the physical, emotional, psychological, and social needs of patients. Nurses are not only involved in treating illnesses but also in promoting health and preventing disease. Their responsibilities extend beyond patient care to include advocacy, education, and collaboration with other healthcare professionals.
Nursing embodies a patient-centered approach, ensuring that care is tailored to individual needs and delivered with respect and compassion. It involves both acute interventions in emergencies and long-term support for chronic conditions, emphasizing continuity of care throughout a patient’s health journey.
Key Areas in Nursing
1. Patient Care
- Overview:
Nurses are central to patient care, providing both direct medical support and emotional reassurance. - Responsibilities:
- Monitoring vital signs and administering medications.
- Assisting with daily activities like mobility, hygiene, and nutrition.
- Managing pain and ensuring patient comfort.
- Settings:
- Hospitals: Intensive care units, emergency rooms, and general wards.
- Clinics: Outpatient care and minor procedures.
- Homes: Providing care for patients recovering from surgery or managing chronic illnesses.
- Impact:
- Enhancing recovery outcomes through diligent monitoring and timely interventions.
2. Specialized Nursing
- Overview:
Specialized nursing focuses on specific patient populations or medical conditions, requiring advanced training and expertise. - Types of Specialized Nursing:
- Pediatric Nursing: Caring for infants, children, and adolescents, addressing growth and developmental needs.
- Geriatric Nursing: Managing the unique challenges of aging, including mobility, dementia, and end-of-life care.
- Psychiatric Nursing: Supporting mental health patients through therapy, medication, and crisis intervention.
- Critical Care Nursing: Providing life-saving care in intensive care units and emergency departments.
- Oncology Nursing: Supporting cancer patients through treatments like chemotherapy and managing symptoms.
- Impact:
- Improving quality of life for patients with complex or specialized needs.
3. Health Education
- Overview:
Nurses play a critical role in educating patients and families about health management and disease prevention. - Responsibilities:
- Teaching patients about medication adherence, wound care, and diet management.
- Conducting community outreach programs on topics like vaccination, hygiene, and lifestyle changes.
- Guiding families on how to care for loved ones with chronic conditions or disabilities.
- Impact:
- Empowering individuals to take control of their health and prevent complications.
Applications of Nursing
1. Delivering Frontline Healthcare Services
- Nurses are often the first point of contact for patients, particularly in emergency and primary care settings.
- Examples:
- Triaging patients in emergency rooms based on the severity of their conditions.
- Administering first aid and stabilizing patients during disasters or accidents.
2. Supporting Medical Teams
- Nurses collaborate closely with doctors, therapists, and other healthcare professionals to provide comprehensive care.
- Examples:
- Assisting surgeons during operations.
- Monitoring post-operative patients and reporting complications to the medical team.
3. Managing Patient Care and Emergencies
- Nurses are trained to handle acute situations, including cardiac arrests, trauma, and respiratory distress.
- Examples:
- Initiating life-saving measures like CPR or defibrillation.
- Coordinating with emergency services during natural disasters or pandemics.
4. Advocating for Patients
- Nurses act as patient advocates, ensuring that individuals receive appropriate care and support.
- Examples:
- Communicating patient concerns to the medical team.
- Ensuring that cultural and personal preferences are respected in treatment plans.
Emerging Trends in Nursing
Telehealth Nursing
- With the rise of digital healthcare, nurses are providing remote consultations and monitoring through telehealth platforms.
Advanced Practice Nursing
- Nurse practitioners (NPs) and clinical nurse specialists (CNSs) are taking on expanded roles in diagnosing and treating illnesses.
Technology Integration
- Nurses are increasingly using electronic health records (EHRs), wearable devices, and AI tools to enhance patient care.
Focus on Mental Health
- The growing awareness of mental health is expanding the role of psychiatric and counseling nurses.
Global Health Nursing
- Nurses are contributing to international health initiatives, addressing issues like infectious diseases, maternal health, and malnutrition.
Challenges in Nursing
Workforce Shortages
- The demand for nurses often exceeds supply, leading to burnout and stress among healthcare providers.
High-Stress Environments
- Nurses frequently work in high-pressure settings, such as emergency rooms and ICUs, requiring resilience and adaptability.
Exposure to Risks
- Nurses are at risk of exposure to infectious diseases, workplace violence, and physical strain.
Balancing Compassion and Professional Boundaries
- Maintaining empathy while managing emotional fatigue can be challenging for long-term care providers.
Future Directions in Nursing
Expanded Roles
- Advanced practice roles like nurse anesthetists and nurse midwives will continue to grow, addressing healthcare gaps.
Focus on Preventive Care
- Nurses will increasingly contribute to public health initiatives, focusing on disease prevention and health promotion.
Integration of AI and Robotics
- Technology will enhance nursing practices, from automated patient monitoring to AI-assisted diagnostics.
Global Collaboration
- Nurses will play a vital role in international health crises and efforts to standardize global health practices.
Education and Specialization
- Continuous professional development and advanced certifications will empower nurses to specialize further and lead healthcare innovations.
Why Study Nursing
Understanding the Core of Patient-Centered Healthcare
Combining Science, Skill, and Compassion
Developing Critical Thinking and Clinical Judgment
Exploring a Diverse and Expanding Profession
Preparing for a Stable, Respected, and Impactful Career
Nursing: Conclusion
Nursing is a cornerstone of healthcare, combining scientific expertise with compassion and empathy to meet the diverse needs of patients. It is a dynamic and evolving field that adapts to advancements in medicine, technology, and societal health needs. Nurses are not only caregivers but also educators, advocates, and leaders who make an immeasurable impact on individual lives and communities. As challenges like aging populations, emerging diseases, and technological changes reshape healthcare, nursing will remain at the forefront of innovation and human connection, ensuring the well-being of future generations.
Frequently Asked Questions – Nursing
What does nursing focus on as a field of study and practice?
Nursing focuses on promoting health, preventing illness, and caring for people across the lifespan who are sick, injured, recovering, or living with chronic conditions. It combines scientific knowledge with compassionate, patient-centred care and teamwork in hospitals, clinics, community settings, and homes.
How is nursing different from medicine?
Medicine focuses mainly on diagnosing and treating disease, while nursing focuses on the person’s overall response to illness, treatment, and life circumstances. Nurses monitor patients closely, provide clinical care and health education, coordinate services, advocate for patients’ needs, and support families as part of a multidisciplinary team.
Why is nursing an important and in-demand career?
Nursing is essential because nurses are often the health professionals who spend the most time with patients and families. They provide continuous monitoring, coordinate care, promote safety, and support recovery and long-term wellbeing. Ageing populations, chronic diseases, and global health challenges mean that qualified nurses are in high demand worldwide.
Which school subjects are most useful if I want to study nursing?
Biology is especially important for understanding the human body, illness, and treatment. Chemistry, mathematics, and general science support drug calculations and evidence-based practice. Subjects that build communication skills, such as languages or humanities, are also helpful for working with patients, families, and healthcare teams.
What personal qualities are important for future nurses?
Future nurses need empathy, patience, and emotional resilience, along with attention to detail and a strong sense of responsibility. Good communication and teamwork skills are vital, as nurses work with patients, families, doctors, and other professionals. Curiosity and commitment to lifelong learning are also important because healthcare keeps changing.
What do students typically learn in a nursing degree?
Nursing students study anatomy and physiology, microbiology, pharmacology, pathophysiology, and nursing theories and assessment. They learn clinical skills such as monitoring vital signs, administering medicines, wound care, communication, documentation, and patient education. Ethics, professional practice, and research skills are also core parts of the curriculum.
What kind of clinical placements do nursing students complete?
Students usually rotate through hospital wards, community and primary care, mental health services, aged care, and sometimes specialist settings such as paediatrics, maternity, or intensive care. Under supervision, they apply classroom learning, practise skills, and learn how different teams deliver care in real-world environments.
What are some main branches and specialisations within nursing?
Major areas include adult or medical-surgical nursing, paediatric nursing, mental health or psychiatric nursing, community and public health nursing, maternity and neonatal nursing, perioperative (theatre) nursing, critical care and emergency nursing. With experience and further study, nurses can also move into advanced or specialist roles.
What is advanced or specialist nursing practice?
Advanced practice nurses, such as nurse practitioners or clinical nurse specialists, have additional education and training that allow them to take on expanded roles. Depending on the country, they may assess and diagnose conditions, order and interpret tests, prescribe some medications, and lead quality improvement or education within healthcare teams.
What challenges do nurses face in their daily work?
Nurses manage busy workloads, changing patient needs, shift work, and emotional situations such as pain, loss, or family stress. They must maintain high standards of safety and infection control, communicate clearly under pressure, and care for their own wellbeing while caring for others, which requires good coping and self-care strategies.
What career paths and workplaces are open to nursing graduates?
Nursing graduates can work in hospitals, clinics, community health centres, schools, aged-care homes, occupational health services, and home-care agencies. Some move into education, research, management, policy, humanitarian and global health work, or roles in health technology and quality improvement.
How does the Nursing page on Prep4Uni.online support my study and career planning?
The Nursing page on Prep4Uni.online introduces key ideas about nursing roles, core sciences, clinical skills, and ethical responsibilities. It helps you connect your current subjects and strengths to university expectations, and gives you a clearer picture of the many directions a nursing qualification can lead in the wider health sector.
Nursing: Review Questions and Answers:
1. What is nursing education and why is it vital for healthcare?
Answer: Nursing education is the comprehensive training process that equips individuals with the skills, knowledge, and clinical competencies required to provide quality patient care. It is vital for healthcare because it ensures that nurses are prepared to meet the complex demands of modern medical environments, from critical care to community health. Through structured programs, nurses learn both theoretical concepts and practical applications, which are essential for maintaining high standards in patient safety and treatment outcomes. Additionally, effective nursing education fosters continuous professional development, which is crucial in an ever-evolving healthcare landscape.
2. How do clinical training programs enhance the competency of nursing students?
Answer: Clinical training programs enhance the competency of nursing students by providing hands-on experience in real-world healthcare settings. These programs allow students to apply theoretical knowledge to practice, developing critical clinical skills under the supervision of experienced professionals. By engaging directly with patients and working in dynamic environments, students build confidence, learn to handle emergencies, and refine their diagnostic abilities. This practical exposure is indispensable for ensuring that graduates are ready to deliver safe, effective, and compassionate care from day one.
3. What role does research play in nursing education and practice?
Answer: Research plays a crucial role in nursing education and practice by advancing the knowledge base and informing evidence-based care. It helps identify best practices, improves patient outcomes, and drives innovations in treatment and care delivery. Through research, nursing professionals can explore new methodologies and technologies that enhance clinical efficiency and quality of care. This commitment to continuous improvement ensures that nursing remains a dynamic field where practice is constantly refined based on the latest scientific evidence.
4. How does compassionate patient care factor into nursing education?
Answer: Compassionate patient care is a cornerstone of nursing education, emphasizing the importance of empathy and ethical practice in healthcare. Nursing programs teach students to not only perform clinical tasks effectively but also to connect with patients on a personal level, which can significantly improve recovery outcomes. This approach ensures that care is patient-centered, addressing both physical and emotional needs. By fostering compassion, nursing education helps build trust between healthcare providers and patients, ultimately leading to higher satisfaction and better overall health.
5. What are the key challenges faced by nursing educators today?
Answer: Nursing educators today face several key challenges, including keeping curriculum content up-to-date with rapid medical advancements and ensuring that teaching methods meet diverse learning needs. They must balance theoretical instruction with practical clinical experience while also addressing the emotional and ethical aspects of patient care. Additionally, technological integration in classrooms and clinical settings requires continuous professional development to stay current with the latest tools and methodologies. These challenges demand innovative solutions and collaborative efforts to ensure that nursing education remains robust and effective in preparing future professionals.
6. How can simulation-based learning improve nursing training?
Answer: Simulation-based learning improves nursing training by providing a safe and controlled environment where students can practice and refine their clinical skills without risking patient safety. Simulations replicate real-life scenarios, enabling learners to experience and respond to emergencies, develop critical thinking, and build confidence in their abilities. This experiential learning method bridges the gap between classroom instruction and clinical practice, ensuring that students are well-prepared for the complexities of healthcare delivery. By incorporating simulation into the curriculum, nursing programs can enhance both competence and readiness for professional practice.
7. How does interprofessional education benefit nursing students?
Answer: Interprofessional education benefits nursing students by fostering collaboration with other healthcare professionals, such as doctors, pharmacists, and therapists. This collaborative learning approach helps students understand the roles and responsibilities of various team members, promoting a more holistic approach to patient care. It encourages communication, teamwork, and shared decision-making, which are critical for effective healthcare delivery. By learning together, students develop mutual respect and a deeper understanding of how to coordinate care, ultimately leading to better patient outcomes and more efficient healthcare systems.
8. What strategies are used to assess student performance in nursing education?
Answer: Strategies used to assess student performance in nursing education include a combination of formative and summative assessments, clinical evaluations, and simulation-based tests. These methods provide a comprehensive picture of a student’s knowledge, practical skills, and professional attitudes. Regular assessments help educators identify areas for improvement and ensure that students are progressing toward competency in both theoretical and clinical aspects. This multi-faceted approach to evaluation is essential for maintaining high standards of care and ensuring that graduates are fully prepared for the demands of the profession.
9. How can mentorship programs enhance the professional growth of nursing students?
Answer: Mentorship programs enhance the professional growth of nursing students by pairing them with experienced practitioners who can provide guidance, support, and real-world insights. Mentors help students navigate the challenges of clinical practice, offer career advice, and model professional behavior. This relationship fosters a deeper understanding of the practical aspects of nursing and encourages the development of critical thinking and problem-solving skills. Through mentorship, students gain confidence, refine their skills, and build a network that supports their long-term career success in the healthcare field.
10. How do advancements in technology influence the future of nursing education and practice?
Answer: Advancements in technology influence the future of nursing education and practice by introducing innovative tools and platforms that enhance both teaching and clinical care. Technologies such as telemedicine, electronic health records, and simulation-based training provide nurses with opportunities to improve patient care and streamline healthcare delivery. These advancements enable more precise, efficient, and personalized learning experiences, ensuring that nurses are well-prepared for the demands of modern healthcare environments. By integrating technology into education and practice, the nursing field can continue to evolve, improving patient outcomes and driving innovation in clinical care.
Nursing: Thought-Provoking Questions and Answers:
1. How might virtual reality (VR) revolutionize clinical training for nursing students?
Answer:
Virtual reality (VR) holds the potential to revolutionize clinical training for nursing students by providing immersive, realistic simulations of patient care scenarios. VR can create a safe learning environment where students can practice procedures, experience emergency situations, and develop critical decision-making skills without any risk to real patients. This technology allows for repeated practice in a controlled setting, enhancing skill acquisition and confidence. Moreover, VR can be used to simulate rare or complex cases that students might not encounter during traditional clinical rotations, thereby broadening their experience and preparedness for a variety of clinical situations.
In addition, VR can facilitate interprofessional education by simulating team-based scenarios that require collaboration among different healthcare professionals. This exposure to multidisciplinary teamwork helps nursing students understand the roles and responsibilities of their colleagues, promoting a more integrated approach to patient care. As VR technology continues to advance, its adoption in nursing education is likely to lead to significant improvements in both teaching methodologies and patient care outcomes, ultimately transforming the future of clinical training.
2. In what ways can artificial intelligence enhance personalized learning in nursing education?
Answer:
Artificial intelligence (AI) can significantly enhance personalized learning in nursing education by tailoring educational content to the individual needs and learning styles of students. AI-powered adaptive learning systems analyze student performance data to identify areas of strength and weakness, allowing educators to customize lesson plans and provide targeted interventions. This personalized approach ensures that each student receives the appropriate level of support, which can lead to improved academic outcomes and greater clinical competence.
Additionally, AI can streamline administrative tasks such as grading and progress tracking, freeing up educators to focus more on direct student engagement and mentorship. By integrating AI into learning management systems, educators can receive real-time feedback on student performance, enabling more responsive and effective instruction. This technological advancement not only improves the efficiency of educational processes but also fosters a more engaging and dynamic learning environment that benefits both students and instructors.
3. How might telehealth and remote clinical training impact nursing education and practice?
Answer:
Telehealth and remote clinical training are transforming nursing education and practice by expanding access to high-quality clinical experiences regardless of geographic constraints. Through telehealth platforms, nursing students can participate in virtual patient consultations, observe remote clinical procedures, and engage with experts in real time, thereby gaining valuable practical insights without the need for physical presence in a hospital setting. This flexibility is particularly beneficial for students in rural or underserved areas, ensuring that they receive comprehensive training despite limited local resources.
Remote clinical training also enables continuous learning and real-time feedback, which can improve clinical skills and decision-making abilities. By integrating digital simulations and virtual case studies, nursing programs can offer a diverse range of scenarios that prepare students for various healthcare challenges. Ultimately, telehealth and remote training methods enhance the overall accessibility, quality, and efficiency of nursing education, contributing to a more robust and adaptable healthcare workforce.
4. What challenges might arise when integrating advanced technology into nursing practice, and how can they be overcome?
Answer:
Integrating advanced technology into nursing practice presents challenges such as high costs, the need for specialized training, and resistance to change from traditional workflows. Nurses may face a steep learning curve when adapting to new digital tools and systems, which can temporarily disrupt patient care and increase the workload. Additionally, technological integration requires significant investment in infrastructure and continuous maintenance, which can strain healthcare budgets, particularly in resource-limited settings.
To overcome these challenges, healthcare institutions must invest in comprehensive training programs that ensure nurses are proficient in using new technologies. Providing ongoing technical support and creating a culture that embraces innovation can help mitigate resistance to change. Moreover, gradually introducing technology through pilot programs and phased implementation can allow for adjustments based on feedback, ensuring a smooth transition. With the right support and planning, the benefits of advanced technology can be fully realized, leading to enhanced patient care and improved operational efficiency.
5. How can nursing education address the growing need for interprofessional collaboration in healthcare?
Answer:
Nursing education can address the growing need for interprofessional collaboration by incorporating interdisciplinary training into the curriculum. Programs that bring together students from various healthcare disciplines, such as medicine, pharmacy, and allied health, create opportunities for collaborative learning and team-based problem-solving. These interprofessional education initiatives foster a deeper understanding of each profession’s roles and responsibilities, leading to improved communication and cooperation in clinical settings.
In addition, simulation-based training and case studies that involve multiple disciplines can help students practice collaborative decision-making in realistic scenarios. This approach not only enhances clinical competence but also prepares future healthcare professionals to work effectively in diverse teams. By emphasizing interprofessional collaboration, nursing education can contribute to the development of a more cohesive and efficient healthcare system that is better equipped to address complex patient needs.
6. How might emerging trends in global health influence the curriculum of nursing education?
Answer:
Emerging trends in global health, such as the rise of chronic diseases, pandemics, and the increasing importance of preventive care, are likely to have a significant impact on the curriculum of nursing education. Nursing programs must adapt by incorporating comprehensive training on global health issues, epidemiology, and public health strategies to prepare future nurses for the challenges of an interconnected world. This evolution in the curriculum will include content on cultural competence, health disparities, and the impact of globalization on healthcare systems, ensuring that nurses are well-equipped to work in diverse settings.
Furthermore, integrating global health perspectives into nursing education encourages students to develop a broader understanding of healthcare beyond their local communities. It promotes the adoption of evidence-based practices and innovative solutions to address global health challenges, ultimately leading to better patient care and improved public health outcomes. As global health trends continue to evolve, nursing curricula must be continuously updated to reflect new challenges and opportunities, fostering a more adaptable and globally informed workforce.
7. What impact does continuing education have on the professional development of nurses?
Answer:
Continuing education has a profound impact on the professional development of nurses by ensuring that they remain current with the latest clinical practices, technological advancements, and research findings. It enables nurses to enhance their skills, update their knowledge, and meet the evolving demands of the healthcare industry. Through ongoing education, nurses can obtain advanced certifications and specializations, which not only improve patient care but also open up new career opportunities and leadership roles.
Furthermore, continuing education fosters a culture of lifelong learning and professional growth, which is essential in a field that is constantly evolving. By staying engaged in professional development activities, nurses are better equipped to adapt to changes, implement evidence-based practices, and contribute to improving healthcare outcomes. This commitment to ongoing learning ultimately enhances the overall quality of care and supports the advancement of the nursing profession.
8. How can cultural competence be integrated into nursing education to improve patient care?
Answer:
Integrating cultural competence into nursing education involves incorporating training that emphasizes understanding and respecting diverse cultural backgrounds and health practices. This approach equips nurses with the skills to effectively communicate with and care for patients from various cultural contexts. By incorporating case studies, simulations, and interactive discussions on cultural diversity, nursing programs can enhance students’ ability to provide empathetic and personalized care, which is crucial for achieving positive patient outcomes.
Moreover, cultural competence training encourages nurses to reflect on their own biases and adapt their care practices to meet the unique needs of each patient. This leads to improved patient satisfaction, better health outcomes, and a reduction in healthcare disparities. As a result, a curriculum that integrates cultural competence not only enriches the educational experience but also plays a critical role in promoting inclusive and effective healthcare practices.
9. How might advancements in simulation technology transform nursing education and clinical training?
Answer:
Advancements in simulation technology are transforming nursing education by providing realistic, immersive environments where students can practice clinical skills without risking patient safety. High-fidelity simulators and virtual reality platforms allow nursing students to engage in hands-on training that mimics real-life medical scenarios, such as emergency responses and routine procedures. This immersive experience helps build confidence, improve technical proficiency, and enhance critical thinking skills, which are essential for effective patient care.
Additionally, simulation technology offers the opportunity for repetitive practice and immediate feedback, enabling students to refine their techniques and correct mistakes in a controlled setting. This iterative learning process not only boosts clinical competence but also prepares nurses for the dynamic challenges of modern healthcare. As simulation technology continues to evolve, its integration into nursing education is likely to lead to more efficient and effective training methods, ultimately improving patient outcomes and safety.
10. How can interprofessional education initiatives improve collaboration between nurses and other healthcare professionals?
Answer:
Interprofessional education initiatives improve collaboration by bringing together students from various healthcare disciplines to learn and work collaboratively. These initiatives expose nursing students to the perspectives and expertise of other professionals, such as physicians, pharmacists, and therapists, fostering mutual respect and understanding. Collaborative learning experiences, such as team-based simulations and interdisciplinary projects, encourage open communication and shared problem-solving, which are essential for effective patient care.
This collaborative approach helps break down traditional silos within healthcare, leading to more cohesive and efficient treatment plans that address the comprehensive needs of patients. By participating in interprofessional education, nurses develop the skills necessary to function as part of a multidisciplinary team, which can enhance patient outcomes and contribute to a more integrated and holistic healthcare system.
11. How might the integration of mobile health applications enhance the delivery of nursing care in clinical settings?
Answer:
The integration of mobile health applications can significantly enhance the delivery of nursing care in clinical settings by providing real-time access to patient data, streamlined communication, and remote monitoring capabilities. Mobile apps enable nurses to quickly access electronic health records, track patient progress, and receive alerts about critical changes in patient conditions. This immediacy enhances decision-making, improves response times, and contributes to more efficient and coordinated patient care.
Furthermore, mobile health applications facilitate better collaboration among healthcare teams by allowing seamless communication between nurses, doctors, and other professionals. They also empower patients to manage their own health through personalized care plans and educational resources. Overall, the use of mobile health technology enhances both the quality and efficiency of nursing care, leading to improved patient outcomes and a more responsive healthcare system.
12. How might ongoing research in nursing science influence future trends in nursing education and practice?
Answer:
Ongoing research in nursing science plays a pivotal role in shaping future trends in nursing education and practice by continually providing new insights into patient care, healthcare delivery, and educational methodologies. Research findings help identify best practices, inform evidence-based teaching strategies, and drive innovations in clinical protocols that enhance patient outcomes. As research advances, it influences curriculum updates, ensuring that nursing education remains current and reflective of the latest scientific developments. This dynamic feedback loop between research and practice is essential for the evolution of the nursing profession.
Moreover, ongoing research promotes a culture of inquiry and continuous improvement within nursing, encouraging professionals to remain curious and committed to lifelong learning. This research-driven approach fosters the development of new technologies, improved treatment methods, and more effective healthcare delivery models. As a result, the integration of cutting-edge research into nursing education not only enhances clinical practice but also ensures that the profession evolves in response to emerging healthcare challenges, ultimately leading to higher standards of patient care and professional excellence.
