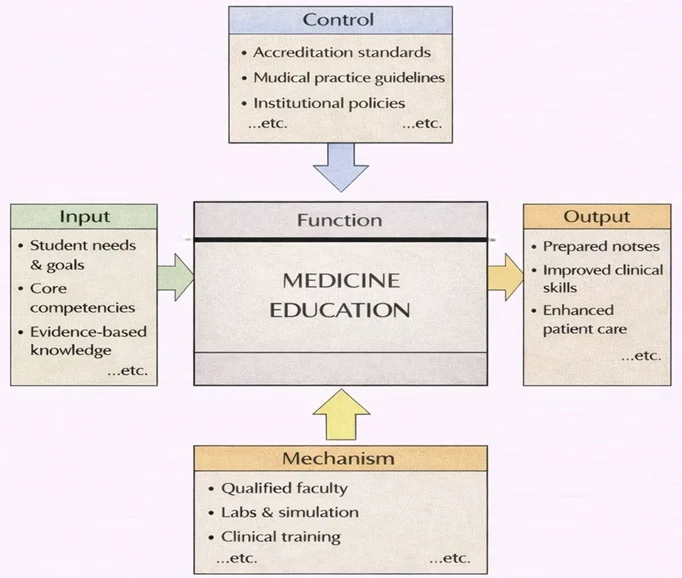
Medicine Education can be viewed as a coordinated system that transforms learner needs into safe, competent clinical practice. As the diagram shows, the process begins with key inputs such as student needs and goals, required medical competencies, and evidence-based scientific knowledge. These inputs are shaped by strong controls—including accreditation requirements, professional medical guidelines, and institutional policies—which set what must be taught, how performance is judged, and what ethical and safety standards must be upheld.
The function is carried out through practical mechanisms: qualified faculty, laboratories and simulation facilities, and supervised clinical training in real healthcare settings. Together, these mechanisms turn knowledge and objectives into lived competence. The intended outputs are clear: prepared medical professionals, stronger clinical skills and judgment, and ultimately improved patient care through consistent, standards-based training.
Medicine is a multidisciplinary field dedicated to the study, diagnosis, treatment, and prevention of diseases. It is both a science and an art, combining evidence-based practices with compassionate care to improve the health and well-being of individuals and communities. Medicine encompasses a vast range of specialties and practices, from primary care to cutting-edge research and surgical innovations, addressing both physical and mental health.
The central focus of medicine is to understand the human body in health and disease, apply this knowledge to alleviate suffering, and promote a better quality of life. As medical science evolves, it integrates new technologies, discoveries, and methodologies, ensuring more accurate diagnoses and effective treatments.

This richly detailed image portrays medicine as an integration of clinical practice and biomedical science. At the center, physicians examine a seated patient, symbolizing diagnosis and patient-centered care. Surrounding them are visual elements of modern medicine: anatomical hearts, a full-body figure highlighting internal systems, DNA strands representing genetics, laboratory test tubes and instruments, and monitor-style graphs indicating vital signs and clinical data. The composition includes classic medical symbols alongside advanced research motifs, emphasizing how medicine draws on biology, technology, and evidence to understand the body, manage disease, and improve wellbeing across individuals and populations.
Table of Contents
Key Areas in Medicine
1. General Medicine
- Definition:
General medicine, or primary care, is the foundation of healthcare, offering comprehensive care for a wide range of conditions and illnesses. - Role:
- Serves as the first point of contact for patients seeking medical attention.
- Focuses on preventive care, early diagnosis, and management of chronic conditions like diabetes, hypertension, and asthma.
- Practitioners:
- General practitioners (GPs) and internists play critical roles in maintaining public health.
2. Specialized Fields
- Medicine includes a broad spectrum of specialties that focus on specific organs, systems, or types of diseases.
- Examples of Specialties:
- Cardiology: The study and treatment of heart and vascular diseases.
- Neurology: Focuses on disorders of the nervous system, including stroke and epilepsy.
- Oncology: The study and treatment of cancers, involving chemotherapy, radiation, and immunotherapy.
- Pediatrics: Care for infants, children, and adolescents, addressing growth, development, and childhood illnesses.
- Dermatology: Deals with skin, hair, and nail conditions.
3. Surgery
- Definition:
Surgery involves operative techniques to treat injuries, diseases, or deformities by manual and instrumental means. - Types of Surgery:
- General Surgery: Focuses on procedures involving the abdomen, skin, and soft tissues.
- Orthopedic Surgery: Treats musculoskeletal issues like fractures and joint disorders.
- Neurosurgery: Involves surgical treatment of brain and spinal cord disorders.
- Minimally Invasive Surgery: Techniques like laparoscopy and robotic surgery that reduce recovery time and risk.
- Role:
- Saves lives in emergencies and enhances quality of life through corrective procedures.
Applications of Medicine
1. Saving Lives
- Medicine directly impacts survival rates through innovations like organ transplantation, advanced surgical techniques, and lifesaving drugs.
- Examples:
- Heart transplants and ventricular assist devices for end-stage heart failure.
- Antiretroviral therapy (ART) for managing HIV/AIDS.
2. Advancing Medical Knowledge
- Research and clinical trials are at the heart of medical progress, leading to breakthroughs in treatment and prevention.
- Examples:
- mRNA vaccines revolutionizing the fight against infectious diseases like COVID-19.
- Development of precision medicine, tailoring treatments based on genetic profiles.
3. Disease Prevention
- Medicine emphasizes preventive care to reduce the burden of disease.
- Examples:
- Vaccination programs eliminating diseases like polio.
- Health education campaigns addressing lifestyle-related conditions such as obesity and smoking.
4. Improving Quality of Life
- Beyond saving lives, medicine aims to enhance the quality of life for patients with chronic or debilitating conditions.
- Examples:
- Pain management and palliative care for terminal illnesses.
- Advanced prosthetics and rehabilitation for amputees.
Emerging Trends in Medicine
Digital Health and Telemedicine
- The integration of digital platforms into healthcare delivery is reshaping how patients interact with medical professionals and access care. Telemedicine—once considered a niche alternative—has now become a mainstream option, particularly after the global push caused by the COVID-19 pandemic. Patients can consult physicians through video conferencing, receive prescriptions electronically, and manage chronic conditions from home without traveling to a clinic.
- Digital health also encompasses mobile apps that track symptoms, medication adherence, mental health, and fitness goals. These tools empower individuals to take a proactive role in their health management and provide real-time data that clinicians can use to tailor treatment plans.
- Examples: Wearable devices such as smartwatches and continuous glucose monitors can now detect changes in heart rate, oxygen saturation, respiratory rate, sleep quality, and even atrial fibrillation. Patients with diabetes benefit from real-time insulin tracking, while individuals at risk for heart disease can monitor vital signs that trigger alerts before a major cardiac event. Telemonitoring systems also assist elderly patients in remote regions, reducing the burden on caregivers and hospitals.
- Digital platforms have also led to the rise of “virtual hospitals,” where multi-disciplinary teams provide continuous care using connected devices and AI-driven dashboards. These models reduce hospital readmission rates and improve outcomes in patients with complex, chronic illnesses.
Artificial Intelligence in Diagnostics
- AI is revolutionizing the accuracy, speed, and scope of medical diagnostics. Machine learning algorithms are now capable of analyzing medical images—such as X-rays, CT scans, and MRIs—with accuracy levels that rival or even surpass trained radiologists. These tools assist physicians by highlighting areas of concern, classifying anomalies, and prioritizing urgent cases.
- In pathology, AI can assess tissue samples for early signs of cancer, identify rare diseases, and suggest diagnoses that may be overlooked by human observers. Predictive analytics use historical data, genetic profiles, and real-time patient information to forecast disease progression and recommend personalized interventions.
- AI also plays a vital role in triage and risk stratification in emergency care. Natural language processing is being used to interpret patient records, lab results, and clinical notes to help doctors make data-informed decisions. Chatbots powered by AI are assisting in pre-diagnosis screening and answering basic medical queries around the clock.
- Hospitals are beginning to implement AI decision-support systems that analyze thousands of data points—from lab tests and medication lists to wearable sensor data—to guide clinicians toward optimal diagnostic pathways. These systems reduce diagnostic errors, cut down unnecessary testing, and shorten time to treatment, particularly in time-sensitive cases like stroke or sepsis.
Gene Editing and CRISPR
- Gene editing, particularly through CRISPR-Cas9 technology, has opened the door to a new era of personalized and precision medicine. This revolutionary approach allows scientists to make highly specific modifications to the DNA of living organisms. In clinical medicine, it is being used to correct genetic defects at their source—offering hope to patients with inherited conditions that were previously untreatable.
- Researchers are exploring applications of gene editing in treating sickle cell anemia, cystic fibrosis, Duchenne muscular dystrophy, and certain cancers. In some clinical trials, patients have seen remarkable improvements after edited immune cells were reintroduced into their bodies to fight leukemia or solid tumors.
- Beyond direct disease treatment, gene editing holds potential for the development of engineered organs, improved organ transplantation, and enhanced resistance to infections. For example, scientists are experimenting with editing the genomes of pigs to make their organs compatible for transplantation into humans—an advancement that could solve the global organ shortage crisis.
- However, CRISPR technologies also raise ethical questions around germline editing and unintended consequences. Regulatory frameworks are evolving to ensure that gene editing is applied responsibly and equitably in clinical contexts. Researchers continue to refine the precision and safety of gene-editing tools to reduce the risk of off-target effects and immune reactions.
Regenerative Medicine
- Regenerative medicine is an interdisciplinary field focused on restoring or replacing damaged cells, tissues, and organs. It harnesses the body’s natural ability to heal and combines it with scientific advancements in cell biology, tissue engineering, and biomaterials. This approach has far-reaching implications in orthopedics, cardiology, neurology, and beyond.
- Stem cell therapies are at the forefront of regenerative innovations. Scientists can now differentiate pluripotent stem cells into specific cell types, such as neurons, cardiomyocytes, or cartilage, and use them to repair injury or degeneration. Clinical trials are exploring how these therapies can treat Parkinson’s disease, spinal cord injuries, heart failure, and Type 1 diabetes.
- Tissue engineering aims to construct biological substitutes for damaged body parts. For instance, researchers are growing skin grafts for burn victims, printing artificial bone using 3D bioprinting techniques, and developing synthetic corneas for patients with vision loss. Advances in scaffold design and bioreactors are helping to mimic the natural microenvironment needed for tissue growth.
- One of the most exciting frontiers is the development of lab-grown organs. Although still in the experimental stage, scientists have successfully created miniature versions of lungs, kidneys, and livers in the laboratory, known as organoids. These models are already being used for drug testing and disease modeling and may eventually replace donor organs in transplantation.
- Regenerative strategies are also being explored for cardiovascular regeneration. In animal studies, researchers have regenerated heart muscle tissue after myocardial infarction, potentially offering alternatives to heart transplants. As technology matures, personalized regenerative therapies based on the patient’s own cells may become standard care for a wide range of degenerative conditions.
Challenges in Medicine
Healthcare Access
- Access to essential medical services remains deeply unequal across different regions, communities, and income groups. In rural and low-income areas, healthcare infrastructure may be severely lacking, with limited availability of hospitals, trained personnel, medications, and diagnostic tools. Even in more developed countries, financial barriers such as high insurance costs or out-of-pocket expenses restrict access for marginalized populations.
- Transportation and geographical isolation further compound access issues, especially for elderly patients and those with chronic conditions who require regular follow-up. In some regions, healthcare deserts—areas with no nearby healthcare providers—leave entire populations without primary care.
- Telemedicine has shown promise in bridging these gaps, but digital inequality (such as limited internet access or digital literacy) can still exclude vulnerable groups. Cultural, linguistic, and social barriers also deter individuals from seeking timely care, particularly in immigrant communities or among those facing stigma related to illness.
- Global health organizations continue to push for universal health coverage, but resource shortages, political instability, and economic disparities hinder progress in many nations.
Antimicrobial Resistance
- The overuse and misuse of antibiotics in both humans and livestock have accelerated the emergence of antimicrobial resistance (AMR), threatening to render many common treatments ineffective. Bacteria are evolving mechanisms to survive even the most potent drugs, leading to infections that are harder and costlier to treat.
- Hospitals around the world are increasingly reporting cases of drug-resistant infections like MRSA (methicillin-resistant Staphylococcus aureus), multi-drug resistant tuberculosis, and carbapenem-resistant Enterobacteriaceae. These “superbugs” increase mortality rates, prolong hospital stays, and demand more complex care.
- Pharmaceutical companies face financial and scientific hurdles in developing new antibiotics, and the global pipeline of next-generation antimicrobials is dangerously thin. Compounding the crisis is the lack of robust regulation and monitoring of antibiotic use in agriculture and aquaculture.
- Public health experts emphasize the need for stronger stewardship programs, better infection control protocols, global surveillance systems, and increased investment in novel therapies to mitigate this looming threat.
Aging Populations
- In many parts of the world, populations are aging rapidly due to improved life expectancy and declining birth rates. As a result, the burden of chronic diseases such as diabetes, cardiovascular disease, arthritis, and dementia is growing, placing immense pressure on healthcare systems and caregivers.
- Older adults often face multiple comorbidities that require complex, long-term, and coordinated care. Managing medication regimens, mobility challenges, mental health issues, and end-of-life decisions becomes more demanding with age.
- Healthcare providers must adapt to the needs of geriatric patients, including investing in specialized gerontology training, elder-friendly hospital design, and community-based support systems that promote independence and dignity.
- Policymakers are also challenged to sustain pension and insurance systems, while preparing for workforce shortages in aged care professions. The intersection of medical, social, and ethical concerns makes aging populations one of the most multifaceted issues in contemporary healthcare.
Ethical Dilemmas
- Rapid advances in biotechnology, artificial intelligence, and genetic engineering have outpaced existing ethical frameworks, raising profound questions about the boundaries of medical practice. Issues like gene editing, embryo selection, cloning, and euthanasia challenge society’s values and legal systems.
- End-of-life decisions, such as physician-assisted dying and withdrawal of life support, are the subject of heated debate around patient autonomy, religious beliefs, and the role of medical professionals. In some countries, these practices are legal under strict conditions, while in others they remain criminalized.
- Consent and data privacy in medical research are also critical concerns, particularly as electronic health records and AI models collect vast quantities of personal health information. Ensuring that patients understand how their data is used, stored, and shared is essential to maintaining trust.
- Equity in access to experimental treatments, clinical trials, or organ transplants remains controversial. Should resources be allocated on a first-come-first-served basis, by need, or by potential benefit? These are not merely theoretical questions but real-world dilemmas that physicians and policymakers face daily.
Why Study Medicine
Understanding the Science of the Human Body and Disease
Making a Lasting Impact on Individual and Public Health
Developing Skills in Critical Thinking, Communication, and Ethics
Exploring a Wide Range of Specializations and Career Paths
Preparing for a Respected and Resilient Profession
Medicine: Conclusion
Medicine is an ever-evolving field that combines science, compassion, and innovation to improve human health. By addressing diseases through prevention, diagnosis, and treatment, it directly impacts lives and shapes the future of societies. The integration of cutting-edge technologies and ongoing research ensures that medicine continues to adapt to emerging challenges and opportunities, fulfilling its core mission to heal, alleviate suffering, and enhance the quality of life for people worldwide.
Frequently Asked Questions – Medicine
What does medicine focus on as a field of study?
Medicine is the study and practice of preventing, diagnosing, and treating disease and injury in humans. It combines scientific knowledge, clinical skills, and ethical judgement to protect health, relieve suffering, and improve quality of life across the lifespan.
How is medicine different from other health-related disciplines?
Medicine focuses on the comprehensive care of individual patients, including diagnosis, treatment, and ongoing management of illness. Other health disciplines, such as nursing, pharmacy, physiotherapy, public health, or biomedical science, often concentrate on specific aspects of care, support, or research. All work together, but the medical doctor typically carries overall responsibility for medical decisions.
Why is medicine considered such a demanding university course?
Medicine is demanding because it requires a strong foundation in the sciences, long hours of study and clinical training, and the ability to make careful decisions that affect people’s lives. Students must integrate complex information, work under pressure, communicate clearly with patients and teams, and maintain high ethical standards over many years of learning and practice.
Which school subjects are most important if I want to apply for medicine?
Most medical schools expect strong performance in biology and chemistry, and many also value physics and mathematics. Subjects that develop critical thinking, communication, and ethical reasoning, such as literature, history, or social studies, can also strengthen your preparation for medical study and patient-focused work.
What personal qualities are important for future doctors?
Future doctors need curiosity and discipline, but also empathy, patience, and integrity. They must be able to listen carefully, explain information clearly, work in teams, and make decisions even when situations are uncertain. Resilience and a commitment to lifelong learning are essential, because medicine keeps evolving.
What do students typically study in the early years of a medical degree?
In the early years, medical students usually study anatomy, physiology, biochemistry, genetics, microbiology, immunology, and pathology. They also begin learning about professionalism, communication skills, medical ethics, and how to take a patient history and perform basic clinical examinations.
What happens during the clinical years of medical training?
During the clinical years, students spend most of their time in hospitals, clinics, and community settings. They rotate through specialties such as internal medicine, surgery, paediatrics, obstetrics and gynaecology, psychiatry, emergency medicine, and general practice. Under supervision, they take histories, examine patients, observe procedures, and learn how teams deliver real-world care.
What are some major branches and specialties within medicine?
Major branches include internal medicine, surgery, paediatrics, obstetrics and gynaecology, psychiatry, family medicine or general practice, emergency medicine, anaesthesiology, radiology, and pathology. Within these, there are many sub-specialties such as cardiology, neurology, oncology, orthopaedics, and intensive care.
How does medical research connect with clinical practice?
Medical research generates evidence about how diseases develop and which tests or treatments work best. Clinicians use this evidence to guide decisions in patient care. Many doctors combine clinical work with research, quality improvement, or teaching, helping to translate new knowledge into safer, more effective practice.
What are some ethical challenges that doctors may face?
Doctors may face ethical questions about consent, confidentiality, resource allocation, end-of-life care, and balancing individual patient needs with public health. They must respect patients’ values and choices, be honest about risks and uncertainties, and follow professional codes and laws designed to protect patients’ rights and dignity.
What career paths are open to medical graduates?
Medical graduates can become hospital doctors, general practitioners, specialists in many clinical fields, public health physicians, medical educators, researchers, health administrators, or advisers in policy and global health. Some work with NGOs, international agencies, or in areas such as occupational or sports medicine.
How does the Medicine page on Prep4Uni.online support my study and career planning?
The Medicine page on Prep4Uni.online helps you understand what medical study involves, from pre-clinical science to clinical rotations and specialties. It links school subjects to university expectations, highlights skills and personal qualities that matter, and supports you in thinking about whether a medical pathway fits your strengths, interests, and long-term goals in health and care.
Medicine: Review Questions and Answers:
1. What is medicine and why is it essential?
Answer: Medicine is the science and practice of diagnosing, treating, and preventing disease, which is essential for preserving human health and improving quality of life. It encompasses a broad range of practices aimed at maintaining and restoring health through the prevention, diagnosis, treatment, and management of illnesses. Medicine plays a critical role in addressing public health challenges and reducing mortality rates worldwide. Its evolution through research and innovation continues to shape effective healthcare delivery and patient care.
2. What are some of the main disciplines within the field of medicine?
Answer: The field of medicine comprises numerous disciplines including internal medicine, surgery, pediatrics, psychiatry, and obstetrics and gynecology, each focusing on different aspects of human health. These specialties work together to provide comprehensive care by addressing various medical conditions and patient needs. Through collaborative efforts, specialists share knowledge and techniques that improve overall treatment outcomes. The diversity of medical disciplines ensures that patients receive the most appropriate and specialized care for their conditions.
3. How does medical research contribute to advancements in treatment?
Answer: Medical research is fundamental to the development of new treatments, diagnostic methods, and preventive strategies that improve patient outcomes. It involves systematic investigation into diseases and therapies, generating evidence that informs clinical practice and healthcare policies. Research drives innovation by uncovering the underlying mechanisms of illness and testing new interventions in controlled settings. As a result, medical research continuously improves the quality of care available and helps extend life expectancy.
4. What role does technology play in modern medicine?
Answer: Technology is a driving force in modern medicine, enhancing diagnostic accuracy, treatment precision, and patient monitoring. Innovations such as digital imaging, robotic surgery, and telemedicine have transformed how healthcare is delivered, making procedures less invasive and more efficient. Technological advancements allow for real-time data analysis and personalized treatment plans that cater to individual patient needs. Overall, the integration of technology in medicine has led to significant improvements in patient care and health outcomes.
5. How do preventive measures and early diagnosis improve patient outcomes?
Answer: Preventive measures and early diagnosis are crucial in reducing the severity and progression of diseases by identifying health issues at an early stage. Regular screenings, vaccinations, and lifestyle interventions can detect potential problems before they escalate, allowing for timely and effective treatment. Early intervention not only improves patient survival rates but also reduces the need for extensive, costly treatments later on. Consequently, these practices enhance overall patient well-being and contribute to a more sustainable healthcare system.
6. What challenges do healthcare professionals face in the practice of medicine?
Answer: Healthcare professionals face a variety of challenges including high patient loads, rapidly evolving medical technologies, and the complexity of managing chronic diseases. They must continuously update their knowledge and skills to keep pace with new research and treatment protocols. Additionally, issues such as administrative burdens, resource limitations, and ethical dilemmas can impact their ability to provide optimal care. Despite these challenges, dedicated healthcare professionals work tirelessly to improve patient outcomes through innovation, collaboration, and ongoing professional development.
7. How do evidence-based practices influence modern medical treatments?
Answer: Evidence-based practices are integral to modern medical treatments as they rely on scientific research and clinical data to guide decision-making. By integrating the best available evidence with clinical expertise, healthcare providers can choose treatments that are proven to be effective. This approach reduces the reliance on anecdotal methods and minimizes the risk of harmful or ineffective interventions. Ultimately, evidence-based practices improve patient outcomes by ensuring that care is both scientifically sound and tailored to individual needs.
8. What is the significance of patient-centered care in medicine?
Answer: Patient-centered care is significant because it prioritizes the individual needs, preferences, and values of patients in the treatment process. This approach fosters a collaborative relationship between patients and healthcare providers, ensuring that decisions are made with the patient’s best interests in mind. By involving patients in their own care, treatment plans are more likely to be followed and adapted to changing circumstances. Patient-centered care not only enhances satisfaction and trust but also leads to improved health outcomes and a better overall quality of life.
9. How do interdisciplinary approaches improve healthcare outcomes?
Answer: Interdisciplinary approaches improve healthcare outcomes by bringing together experts from various fields such as medicine, nursing, psychology, and social work to address complex health issues holistically. This collaborative model ensures that patients receive comprehensive care that considers multiple aspects of their health and well-being. By integrating diverse perspectives, interdisciplinary teams can develop more effective treatment plans and provide coordinated care that addresses both physical and mental health. As a result, patients benefit from more well-rounded and efficient healthcare services.
10. How is public health integrated into the field of medicine?
Answer: Public health is integrated into medicine through initiatives that focus on disease prevention, health promotion, and community well-being. Medical professionals work alongside public health experts to identify health trends, implement vaccination programs, and promote healthy behaviors. This integration ensures that individual patient care is complemented by broader efforts to reduce the incidence of diseases and improve population health. By combining clinical practice with public health strategies, the overall effectiveness of healthcare systems is enhanced, leading to improved health outcomes on a large scale.
Medicine: Thought-Provoking Questions and Answers:
1. How might advancements in genomics and personalized medicine revolutionize future treatment protocols?
Answer:
Advancements in genomics and personalized medicine are poised to revolutionize future treatment protocols by allowing healthcare providers to tailor therapies based on individual genetic profiles. As researchers decode the human genome and understand the genetic underpinnings of diseases, treatments can be customized to target specific mutations or biological pathways, resulting in higher efficacy and fewer side effects. This personalized approach not only improves patient outcomes but also paves the way for preventive strategies that anticipate and mitigate potential health issues before they manifest. Ultimately, the integration of genomics into clinical practice represents a significant step towards more precise, individualized healthcare that is both cost-effective and transformative.
In addition, these advancements facilitate the development of targeted pharmaceuticals and gene therapies that address previously untreatable conditions. As personalized medicine continues to evolve, it will likely lead to a paradigm shift in healthcare, where treatment plans are designed with a deep understanding of each patient’s unique genetic makeup. This shift promises to enhance the overall quality of care and drive significant improvements in public health, marking a new era in medical innovation and patient-centered treatment.
2. In what ways can artificial intelligence (AI) transform diagnostic accuracy and treatment outcomes in medicine?
Answer:
Artificial intelligence (AI) has the potential to transform diagnostic accuracy and treatment outcomes by leveraging advanced algorithms to analyze complex medical data. AI systems can quickly process vast amounts of patient data, including imaging, genetic information, and electronic health records, to identify patterns that may indicate early signs of disease. This capability leads to faster, more accurate diagnoses and allows for timely interventions, which are crucial for effective treatment. As a result, AI enhances patient care by reducing diagnostic errors and enabling more personalized treatment plans.
Moreover, AI-driven predictive models can forecast disease progression and treatment responses, helping clinicians tailor interventions to individual needs. By integrating AI into healthcare, medical professionals can optimize resource allocation, improve operational efficiency, and ultimately achieve better patient outcomes. The transformative power of AI in medicine lies in its ability to augment human expertise, leading to a more proactive and precise approach to healthcare delivery.
3. How can telemedicine reshape access to quality healthcare in remote or underserved communities?
Answer:
Telemedicine reshapes access to quality healthcare in remote or underserved communities by bridging the gap between patients and healthcare providers through digital communication tools. It enables individuals in geographically isolated areas to consult with specialists, receive timely diagnoses, and access follow-up care without the need for extensive travel. This increased accessibility not only improves health outcomes but also reduces the financial and logistical barriers that often prevent patients from obtaining necessary medical services. By providing virtual consultations and remote monitoring, telemedicine can deliver comprehensive care in a cost-effective and efficient manner.
Furthermore, telemedicine facilitates continuous care by enabling regular check-ups and real-time monitoring of chronic conditions. Digital platforms allow for the collection and analysis of health data, which can be used to customize treatment plans and improve patient management. As telemedicine becomes more integrated into healthcare systems, it holds the promise of reducing disparities in healthcare access, enhancing the quality of life for underserved populations, and ultimately contributing to a more equitable and resilient health system.
4. What ethical considerations arise from the use of emerging medical technologies, and how can they be addressed?
Answer:
The use of emerging medical technologies raises several ethical considerations, including patient privacy, informed consent, and equitable access to advanced treatments. As digital health tools and genomic therapies become more prevalent, ensuring that patient data is securely stored and used responsibly is paramount. There is also the challenge of ensuring that patients fully understand the implications of new technologies, which requires clear communication and robust consent processes. Addressing these ethical concerns involves establishing stringent regulatory frameworks and ethical guidelines that govern the use of such technologies.
Additionally, ensuring equitable access to advanced medical technologies is crucial to prevent widening disparities in healthcare. Policymakers must work to create systems that provide all patients, regardless of socioeconomic status, with access to innovative treatments. This may involve subsidizing costs, providing public funding, and promoting transparency in healthcare practices. By proactively addressing these ethical issues, the medical community can harness the benefits of emerging technologies while safeguarding patient rights and promoting social justice.
5. How might the integration of interdisciplinary research improve patient outcomes in modern medicine?
Answer:
The integration of interdisciplinary research in modern medicine can lead to significant improvements in patient outcomes by fostering a more comprehensive understanding of health and disease. By combining insights from fields such as biology, engineering, data science, and psychology, researchers can develop innovative diagnostic tools and treatment methods that address complex medical challenges. This collaborative approach enables the development of holistic interventions that consider multiple dimensions of patient health, leading to more effective and personalized care.
Interdisciplinary research also promotes the sharing of best practices and knowledge across diverse fields, which can drive innovation and accelerate the translation of scientific discoveries into clinical practice. For example, advancements in biomedical engineering can lead to the creation of more effective medical devices, while data science can optimize treatment protocols through predictive analytics. The resulting synergy not only enhances the quality of care but also contributes to the overall advancement of medical science, ultimately improving patient outcomes and quality of life.
6. How can medical professionals balance the rapid pace of technological innovation with the need for evidence-based practice?
Answer:
Balancing rapid technological innovation with the need for evidence-based practice requires medical professionals to adopt a critical and methodical approach to integrating new technologies into clinical care. This involves rigorous evaluation of emerging tools through clinical trials, systematic reviews, and pilot studies to ensure that they are both safe and effective. By adhering to evidence-based protocols, practitioners can make informed decisions that prioritize patient well-being while embracing innovation.
Furthermore, continuous professional development and collaboration among clinicians, researchers, and industry experts are essential for staying abreast of technological advancements. This collaborative environment fosters an ongoing dialogue about best practices and emerging trends, allowing healthcare providers to integrate new technologies gradually and responsibly. Ultimately, this balanced approach ensures that innovations enhance, rather than compromise, the quality of care delivered to patients.
7. How might advances in genomics contribute to the development of personalized medicine in the near future?
Answer:
Advances in genomics are paving the way for personalized medicine by enabling the identification of genetic markers that influence disease susceptibility and treatment response. With the increasing affordability and accessibility of genomic sequencing, healthcare providers can now tailor treatments to individual genetic profiles, optimizing therapeutic efficacy and minimizing adverse effects. This personalized approach not only improves patient outcomes but also reduces the trial-and-error aspect of traditional treatment methods, leading to more efficient and targeted interventions.
Moreover, genomic research facilitates the discovery of new biomarkers and drug targets, which can lead to the development of novel therapies and precision medicine approaches. As our understanding of the human genome deepens, personalized medicine will become increasingly integrated into routine clinical practice, offering customized treatment plans that address the unique genetic makeup of each patient. This evolution represents a significant shift in healthcare, moving towards more individualized and predictive approaches to disease management.
8. What are the potential economic impacts of integrating advanced technologies into healthcare systems?
Answer:
Integrating advanced technologies into healthcare systems has the potential to generate significant economic benefits by improving efficiency, reducing costs, and enhancing patient outcomes. Technologies such as telemedicine, AI-driven diagnostics, and robotic surgery can streamline clinical workflows, reduce hospital stays, and lower the incidence of medical errors. These improvements can lead to substantial cost savings for healthcare providers and patients alike, making advanced care more accessible and affordable.
On the other hand, the initial investment required for implementing cutting-edge technologies can be considerable, posing challenges for resource-limited healthcare systems. However, as technology adoption increases and becomes more widespread, economies of scale are likely to drive down costs, ultimately resulting in a more sustainable and cost-effective healthcare model. The long-term economic impacts include not only improved health outcomes and reduced healthcare expenditures but also enhanced productivity and a more resilient healthcare infrastructure.
9. How can patient engagement be enhanced through digital health solutions, and what are the potential benefits?
Answer:
Digital health solutions enhance patient engagement by providing accessible platforms for communication, education, and self-management of health. Tools such as mobile apps, online portals, and wearable devices empower patients to monitor their health, receive personalized recommendations, and track their progress in real time. This increased engagement leads to better adherence to treatment plans, timely interventions, and ultimately improved health outcomes. Digital solutions also offer interactive features that can motivate patients to take an active role in managing their well-being, creating a more collaborative relationship between patients and healthcare providers.
In addition, enhanced patient engagement through digital platforms can lead to more informed decision-making and higher satisfaction with care. When patients have access to comprehensive health information and resources, they can better understand their conditions and treatment options. This proactive involvement not only fosters better clinical outcomes but also reduces the overall burden on the healthcare system by minimizing unnecessary visits and promoting preventive care.
10. How might public health initiatives leverage data analytics to improve population health outcomes?
Answer:
Public health initiatives can leverage data analytics to improve population health outcomes by systematically collecting and analyzing health data from diverse sources. Data analytics enables the identification of trends, risk factors, and emerging health issues, allowing public health officials to target interventions more effectively. By analyzing data on disease prevalence, vaccination rates, and health behaviors, policymakers can design evidence-based programs that address the specific needs of different communities, ultimately leading to better health outcomes.
Furthermore, data analytics supports real-time monitoring and evaluation of public health initiatives, facilitating timely adjustments and resource allocation. This approach not only improves the efficiency of health interventions but also enhances the ability to predict and respond to public health crises. As a result, the strategic use of data analytics can transform public health efforts, ensuring that initiatives are both proactive and impactful, leading to a healthier population overall.
11. How might emerging trends in telemedicine influence the future of healthcare delivery and patient outcomes?
Answer:
Emerging trends in telemedicine are set to reshape healthcare delivery by expanding access to medical care, especially in remote and underserved areas. Telemedicine platforms facilitate virtual consultations, remote monitoring, and digital health assessments, enabling patients to receive timely care without the need for physical visits to healthcare facilities. This shift not only improves accessibility but also enhances patient outcomes by ensuring continuous monitoring and early intervention in managing chronic conditions. The integration of telemedicine into mainstream healthcare promotes efficiency, reduces healthcare costs, and improves overall service delivery.
Moreover, telemedicine fosters a more patient-centered approach by offering flexible scheduling and personalized care plans. As technology advances, the quality of virtual care is expected to improve, leading to better diagnostic accuracy and treatment efficacy. This evolution in healthcare delivery has the potential to transform patient experiences, making healthcare more proactive, accessible, and tailored to individual needs, which ultimately leads to improved long-term health outcomes.
12. How can interdisciplinary collaboration drive innovation and improve healthcare practices in modern medicine?
Answer:
Interdisciplinary collaboration is essential for driving innovation and improving healthcare practices by integrating diverse expertise from fields such as medicine, engineering, data science, and public health. This collaborative approach encourages the development of comprehensive solutions that address complex medical challenges, leading to more effective and efficient patient care. By pooling knowledge from different disciplines, healthcare professionals can create innovative treatment protocols, advanced diagnostic tools, and more robust preventive strategies that improve overall health outcomes.
Such collaboration also fosters a culture of continuous learning and adaptability, enabling healthcare systems to remain responsive to emerging challenges and technological advancements. For example, interdisciplinary teams can work together to develop AI-driven platforms that enhance diagnostic accuracy or design digital health solutions that improve patient engagement. Ultimately, interdisciplinary collaboration not only accelerates the pace of innovation but also ensures that healthcare practices are holistic, evidence-based, and capable of meeting the diverse needs of patients in a rapidly evolving medical landscape.
