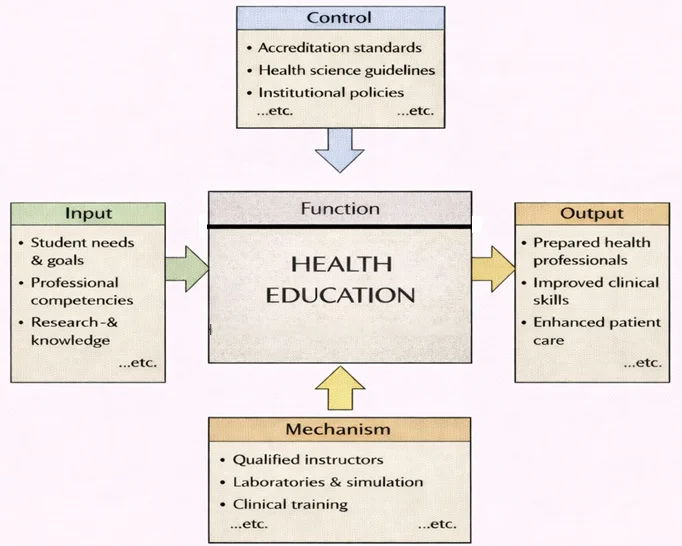
Health Education can be viewed as a structured system that turns learning needs into real-world healthcare capability. On the input side, it begins with student needs and goals, the professional competencies learners must master, and the research-based knowledge that underpins modern practice. This function is shaped by clear controls—accreditation standards, health science guidelines, and institutional policies—which set the boundaries for what must be taught, how quality is judged, and what ethical or safety requirements must be met. The transformation happens through practical mechanisms: qualified instructors, laboratories and simulation environments, and supervised clinical training. When these parts work together, the outputs are not just “graduates,” but prepared health professionals with stronger clinical skills—ultimately contributing to safer, more effective, and more compassionate patient care.
Welcome to the Health section of Prep4Uni.online — your trusted learning hub for exploring pathways in healthcare, medicine, wellness, public health, and rehabilitation sciences. Whether you’re pursuing a career in clinical practice, population health, or sports science, this section equips you with knowledge, skills, and real-world applications essential for personal growth and societal impact.
Health and medical sciences are pivotal in enhancing individual well-being and community vitality. From preventing diseases and delivering therapeutic care to advancing fitness and rehabilitation outcomes, the disciplines within health sciences offer diverse and rewarding opportunities.

This vivid image presents health as a blend of clinical care, scientific understanding, and everyday habits. A doctor and medical symbols (crosses, charts, and lab flasks) represent diagnosis, treatment, and research, while large DNA helices highlight genetics and modern biomedical science. In the center and foreground, figures run, cycle, and lift weights, emphasizing physical activity, prevention, and fitness. Heartbeat lines and monitoring-style graphics suggest measurement and health analytics, tying together personal behavior, medical technology, and evidence-based decisions. Overall, the scene conveys health as a whole-system idea—body, mind, environment, and care working in balance.
Choose a Doorway into Health
Medicine
Explore clinical reasoning, patient care, and the science behind diagnosis and treatment.
Nursing
Develop compassionate, evidence-based practice across community and acute settings.
Pharmacy
Learn pharmacology, therapeutics, and safe medication management for diverse populations.
Public Health
Prevent disease and advance equity through data, policy, and community action.
Dentistry
Combine biomedical science and clinical skill to protect oral health and confidence.
Veterinary Science
Care for animals and safeguard public health across species and ecosystems.
Sports Science
Optimize performance with biomechanics, physiology, and evidence-based coaching.
Physical Education
Teach movement skills and lifelong fitness with inclusive, safe practice.
Kinesiology
Study human movement to prevent injury and enhance function across the lifespan.
Physiotherapy
Rehabilitate and restore mobility through assessment, exercise, and hands-on care.
See the Bigger Picture
STEM
Connect health with biotech, data science, and medical devices.
Humanities & Social Sciences
Center ethics, equity, and cultural competence in care.
Business, Economics & Law
Navigate health systems, policy, and the economics of care.
Education
Advance patient education, coaching, and workforce development.
Arts, Design & Media
Communicate health clearly with design, media, and storytelling.
Table of Contents
Key Areas of Focus in Health and Medical Sciences
Healthcare and Clinical Practice
Diagnose, treat, and prevent a wide range of illnesses and injuries.
Improve patient outcomes through evidence-based interventions and patient-centered care.
Explore specialties across medicine, nursing, pharmacy, allied health, and therapeutic disciplines.
Public and Community Health
Promote health literacy and well-being through education and policy.
Develop community-based prevention programs that address health inequalities.
Engage in global and environmental health initiatives that influence populations at scale.
Physical Health and Rehabilitation Sciences
Improve physical fitness, movement efficiency, and athletic performance.
Support injury recovery and optimize functional ability through physiotherapy and kinesiology.
Contribute to preventive care in sports medicine and physical education.
Practical Applications of Health Disciplines
Deliver healthcare in hospitals, clinics, community centers, and telehealth settings.
Conduct research and innovation in biomedical sciences and pharmaceuticals.
Design health education campaigns and policy frameworks to reduce disease burden.
Apply sports science to coaching, rehabilitation, and performance optimization.
Core Skills Developed in Health Education
Engaging in health and medical training cultivates transferable skills including:
Clinical reasoning and diagnostic skills
Scientific literacy and analytical thinking
Patient communication and empathy
Public health planning and program design
Interdisciplinary collaboration and ethics in care
Lifelong Relevance of Health Education Beyond University
The competencies developed in health education extend far beyond academic environments. They support:
Career adaptability in healthcare, wellness, and research sectors
Ongoing professional development through certifications and specializations
Personal empowerment to make informed health and lifestyle choices
Contributions to healthier workplaces, families, and communities
Examples of Disciplines
1. Medicine
- Focus: The study and practice of diagnosing, treating, and preventing diseases.
- Key Areas:
- General medicine: Primary care for a wide range of conditions.
- Specialized fields: Cardiology, neurology, oncology, pediatrics, and more.
- Surgery: Operative techniques to treat injuries or illnesses.
- Applications:
- Saving lives through innovative treatments and procedures.
- Advancing medical knowledge through research and clinical trials.
2. Nursing
- Focus: Providing compassionate care to patients, managing recovery, and promoting health.
- Key Areas:
- Patient care: Monitoring and assisting with recovery in hospitals, clinics, and homes.
- Specialized nursing: Pediatric, geriatric, psychiatric, and critical care.
- Health education: Teaching patients and families about preventive care.
- Applications:
- Delivering frontline healthcare services.
- Supporting medical teams in managing patient care and emergencies.
3. Pharmacy
- Focus: The preparation, dispensing, and study of medications.
- Key Areas:
- Pharmacology: Understanding how drugs interact with the body.
- Pharmaceutical chemistry: Developing new drugs and formulations.
- Clinical pharmacy: Advising healthcare teams on drug therapies.
- Applications:
- Ensuring the safe and effective use of medications.
- Researching new treatments for diseases.
4. Public Health
- Focus: Protecting and improving community health through policies, education, and preventive programs.
- Key Areas:
- Epidemiology: Studying disease patterns and outbreaks.
- Health policy: Developing strategies for healthcare systems.
- Community health: Educating populations about wellness and prevention.
- Applications:
- Managing public health crises such as pandemics.
- Reducing health disparities through targeted interventions.
5. Dentistry
- Focus: Oral health, including the diagnosis and treatment of teeth, gums, and mouth conditions.
- Key Areas:
- General dentistry: Routine care like cleaning, fillings, and extractions.
- Orthodontics: Correcting teeth alignment and jaw structure.
- Periodontology: Treating gum diseases and supporting oral health.
- Applications:
- Improving oral hygiene and preventing dental diseases.
- Enhancing smiles through cosmetic dentistry.
6. Veterinary Science
- Focus: The medical care of animals, including pets, livestock, and wildlife.
- Key Areas:
- Animal surgery: Treating injuries and conditions in animals.
- Preventive care: Vaccinations, parasite control, and nutrition.
- Research: Studying zoonotic diseases and improving animal health.
- Applications:
- Ensuring the health of companion animals and livestock.
- Protecting public health by controlling animal-borne diseases.
7. Sports Science
- Focus: Enhancing athletic performance and understanding the physiological impact of exercise.
- Key Areas:
- Biomechanics: Analyzing movement and physical performance.
- Exercise physiology: Studying the body’s responses to physical activity.
- Sports psychology: Improving mental resilience and focus in athletes.
- Applications:
- Optimizing training programs for professional athletes.
- Developing rehabilitation strategies for sports injuries.
8. Physical Education
- Focus: Teaching and promoting physical activity, fitness, and wellness.
- Key Areas:
- Curriculum development: Designing fitness programs for schools and communities.
- Coaching: Training individuals and teams for recreational and competitive sports.
- Fitness assessment: Evaluating physical performance and health metrics.
- Applications:
- Encouraging lifelong fitness habits.
- Supporting community health through active lifestyles.
9. Kinesiology
- Focus: The study of human movement and its impact on health and performance.
- Key Areas:
- Motor control: Understanding how the brain and body coordinate movements.
- Rehabilitation: Restoring mobility and function after injuries.
- Performance enhancement: Improving strength, flexibility, and endurance.
- Applications:
- Designing ergonomic solutions for workplaces.
- Supporting physical therapy and sports training programs.
10. Physiotherapy
- Focus: Restoring movement and managing pain through therapeutic exercises and techniques.
- Key Areas:
- Orthopedic physiotherapy: Treating musculoskeletal injuries.
- Neurological physiotherapy: Managing conditions like strokes and Parkinson’s disease.
- Pediatric physiotherapy: Assisting children with developmental challenges.
- Applications:
- Helping patients recover from surgeries and injuries.
- Improving quality of life for individuals with chronic conditions.
Future Trends and Emerging Directions in Health Sciences
Stay future-ready by exploring how global health landscapes are evolving:
Artificial intelligence in diagnostics and personalized medicine
Telehealth and digital health technologies
Genomic medicine and precision healthcare
Sustainable healthcare systems and environmental health links
Global pandemic preparedness and mental health advocacy
Conclusion: Your Health Education Journey Starts Here
At Prep4Uni.online, we believe a strong foundation in health sciences empowers individuals and transforms communities. Explore our curated resources, stay updated with innovations, and pursue a meaningful career in healthcare, medicine, and public health. Begin your journey toward impact and excellence today.
Frequently Asked Questions – Health Hub
What does the Health hub on Prep4Uni.online focus on?
The Health hub on Prep4Uni.online introduces you to how health is studied from multiple angles, including medicine, nursing, public health, mental health, health policy, and health promotion. It helps you see how biological, psychological, social, and environmental factors interact to shape health across the lifespan.
What is the difference between health, health sciences, and medicine?
Health is a broad concept that includes physical, mental, and social wellbeing. Health sciences study the mechanisms behind health and disease, using biology, chemistry, statistics, psychology, and social sciences. Medicine is a professional field focused on diagnosing, treating, and preventing disease in individual patients, drawing on health sciences but with a strong clinical emphasis.
Why is it important to study health before university?
Studying health before university helps you understand how bodies work, how illnesses develop, and how lifestyle, environment, and inequality affect people’s wellbeing. It also prepares you for health-related degrees by building scientific literacy, critical thinking, empathy, and an awareness of ethical and policy debates in healthcare.
Which school subjects are useful for health-related university courses?
Core subjects for many health degrees include biology and chemistry, with mathematics or statistics often recommended. Physics can be helpful for fields like medical imaging or biomedical engineering. Humanities and social sciences are also valuable, especially for public health, health policy, psychology, and global health.
What is the difference between clinical and non-clinical health careers?
Clinical careers, such as doctor, nurse, physiotherapist, or pharmacist, involve direct contact with patients and responsibility for diagnosis, treatment, or ongoing care. Non-clinical careers, such as public health analyst, health educator, policy officer, researcher, or health administrator, focus on research, planning, systems, and population-level health rather than individual patient care.
How does public health differ from individual healthcare?
Individual healthcare focuses on diagnosing and treating single patients, while public health focuses on preventing disease and promoting health in populations. Public health uses tools such as surveillance, epidemiology, vaccination programmes, health promotion campaigns, and policy interventions to reduce risks and improve wellbeing at community, national, or global levels.
Why are mental health and wellbeing important parts of the Health hub?
Mental health and wellbeing are essential to how people function, learn, work, and build relationships. The Health hub recognises that mental health is not separate from physical health: stress, trauma, and social conditions can affect the body, and physical illness can affect mood and thinking. Understanding mental health is important for many health and education careers.
How do social and economic factors influence health?
Health is shaped not only by biology and behaviour, but also by social and economic conditions such as income, housing, work, education, gender, and discrimination. These “social determinants of health” help explain why some groups experience higher rates of illness and shorter life expectancy, even when healthcare services are available.
What role do data, statistics, and evidence play in health fields?
Data and evidence are central to health because they help professionals understand patterns of disease, evaluate treatments, and design effective interventions. Skills in statistics, critical reading of research, and evidence-based decision making are important in clinical practice, public health, health policy, and health management.
How are technology and innovation changing health and healthcare?
Technology and innovation are transforming health through telemedicine, electronic health records, wearable devices, AI-supported diagnostics, personalised medicine, and new medical devices. These tools can improve access and quality of care, but they also raise questions about privacy, equity, and the need for human judgement and compassion.
What kinds of careers can grow from an interest in health?
An interest in health can lead to many careers, including medicine, nursing, allied health professions, pharmacy, public health, health promotion, epidemiology, health economics, global health, health policy and management, biomedical research, mental health services, and roles in NGOs or international organisations focused on health.
How does the Health hub on Prep4Uni.online support my study and career planning?
The Health hub on Prep4Uni.online connects scientific foundations with social, psychological, and policy perspectives on health. It helps you explore different health disciplines, understand university expectations, and think about how your strengths and interests could fit into clinical or non-clinical health careers, locally and globally.
Health: Review Questions and Answers:
1. What is the significance of health education in modern society?
Answer: Health education plays a crucial role in modern society by empowering individuals with the knowledge and skills to make informed decisions about their well-being. It helps people understand the importance of preventive care, proper nutrition, and regular exercise, which can lead to healthier lifestyles and reduced medical costs. Effective health education also promotes awareness about chronic diseases and mental health issues, encouraging early intervention and treatment. By providing reliable health information, it supports a more resilient and informed community, ultimately contributing to improved public health outcomes.
2. How does preventive care contribute to overall well-being?
Answer: Preventive care is essential for overall well-being as it focuses on the early detection and management of potential health issues before they become severe. Regular check-ups, screenings, and vaccinations can help identify diseases at an early stage, leading to more effective treatment and lower healthcare costs. By emphasizing prevention, individuals can maintain a higher quality of life and reduce the risk of chronic illnesses. This proactive approach not only improves individual health outcomes but also alleviates the burden on healthcare systems by minimizing emergency care and long-term treatments.
3. What role does mental health play in physical well-being?
Answer: Mental health is integral to physical well-being as the two are deeply interconnected, with each influencing the other. Good mental health supports emotional stability, which in turn contributes to better physical health by reducing stress and promoting healthier lifestyle choices. Conversely, poor mental health can lead to physical issues such as chronic stress, sleep disturbances, and weakened immunity. Recognizing and addressing mental health concerns is vital for a holistic approach to health, ensuring that both mind and body are supported for overall wellness.
4. How do modern medical trends influence patient care?
Answer: Modern medical trends, such as the adoption of digital health technologies and personalized medicine, are significantly transforming patient care. These trends facilitate more accurate diagnoses, streamlined treatments, and improved patient monitoring through innovative tools and data analytics. They allow healthcare providers to tailor treatments to individual needs, enhancing the effectiveness of interventions and improving patient outcomes. As a result, patients benefit from a more responsive, efficient, and patient-centered healthcare system that continually evolves to meet contemporary health challenges.
5. What is the importance of nutrition in maintaining overall health?
Answer: Nutrition is a cornerstone of overall health, as it provides the essential nutrients required for bodily functions and disease prevention. A balanced diet supports immune function, enhances energy levels, and contributes to the proper growth and repair of tissues. Adequate nutrition also plays a significant role in preventing chronic diseases such as obesity, diabetes, and heart disease. By promoting healthy eating habits and providing education on nutritional values, individuals can improve their quality of life and reduce their risk of developing long-term health issues.
6. How does regular physical activity contribute to health and wellness?
Answer: Regular physical activity is vital for maintaining health and wellness because it strengthens the cardiovascular system, improves muscle tone, and enhances flexibility. It helps regulate weight, reduces the risk of chronic diseases, and boosts overall energy levels. Physical activity also has positive effects on mental health by reducing stress, anxiety, and symptoms of depression, while promoting a sense of well-being. Incorporating exercise into daily routines leads to a more balanced and healthy lifestyle, supporting both physical and emotional health.
7. What benefits do regular health screenings offer to individuals?
Answer: Regular health screenings offer numerous benefits by enabling early detection of potential health issues, which can lead to more effective and less invasive treatments. They provide critical information about an individual’s health status, allowing for timely interventions and better management of chronic conditions. Health screenings also serve as an opportunity for educators and healthcare providers to deliver preventive care advice and promote healthy lifestyle changes. Ultimately, these screenings contribute to improved long-term health outcomes and a reduction in overall healthcare costs.
8. How can technology improve access to healthcare services?
Answer: Technology improves access to healthcare services by bridging geographical and economic barriers, making it easier for individuals to receive timely care. Telemedicine, online consultations, and mobile health apps allow patients to connect with healthcare providers from the comfort of their homes, reducing the need for travel and minimizing waiting times. These technological advancements also facilitate the monitoring of chronic conditions and the delivery of personalized care. As a result, technology plays a critical role in expanding healthcare access and enhancing the quality of care for underserved populations.
9. What challenges does the current healthcare system face, and how can they be addressed?
Answer: The current healthcare system faces challenges such as rising costs, unequal access to services, and the burden of chronic diseases, which strain resources and impact quality of care. There is also the issue of integrating rapidly evolving technology with existing infrastructures. Addressing these challenges requires a multifaceted approach that includes policy reform, increased funding for preventive care, and the adoption of innovative technologies. Collaborative efforts among governments, healthcare providers, and communities are essential to create a more efficient, equitable, and sustainable healthcare system.
10. How do public health initiatives contribute to community well-being?
Answer: Public health initiatives contribute significantly to community well-being by promoting preventive care, reducing the spread of diseases, and ensuring that vital health services are accessible to all. These initiatives often include vaccination programs, health education campaigns, and community-based interventions that target specific health challenges. By focusing on prevention and early intervention, public health efforts help reduce healthcare costs and improve the overall quality of life for community members. In addition, these programs foster a culture of health and wellness that can lead to long-term improvements in public health outcomes.
Health: Thought-Provoking Questions and Answers:
1. How might emerging digital health technologies transform the future of healthcare delivery?
Answer:
Emerging digital health technologies such as wearable devices, telemedicine, and AI-driven diagnostics are set to revolutionize healthcare delivery by providing real-time monitoring and personalized care. These technologies enable continuous health tracking, which can lead to early detection of medical conditions and timely interventions, ultimately improving patient outcomes. They also facilitate remote consultations, reducing the need for physical visits to healthcare facilities and making healthcare more accessible, especially for individuals in rural or underserved areas. The integration of these tools into the healthcare system is likely to lead to a more proactive and patient-centered approach, reshaping traditional models of care.
Furthermore, digital health technologies promote data-driven decision-making by providing vast amounts of patient data that can be analyzed to optimize treatment plans and predict health trends. This transformation not only enhances the efficiency and accuracy of healthcare services but also reduces costs by minimizing unnecessary hospital visits and procedures. As these technologies continue to advance, they will play a pivotal role in creating a more responsive and sustainable healthcare system that adapts to the needs of a diverse patient population.
2. What are the potential impacts of personalized medicine on healthcare outcomes?
Answer:
Personalized medicine, which tailors medical treatment to the individual characteristics of each patient, has the potential to significantly improve healthcare outcomes by ensuring that treatments are more effective and have fewer side effects. This approach uses genetic, environmental, and lifestyle information to develop targeted therapies that address the specific needs of patients. As a result, personalized medicine can lead to higher success rates in treating complex diseases, such as cancer and chronic illnesses, by focusing on interventions that are most likely to be effective for each individual.
The benefits of personalized medicine extend beyond treatment efficacy; they also include improved patient satisfaction and reduced healthcare costs over time. By optimizing treatment plans and reducing trial-and-error approaches, personalized medicine can decrease the overall burden on the healthcare system. However, implementing personalized medicine on a broad scale requires significant investments in research, technology, and data infrastructure, as well as addressing ethical and privacy concerns related to the use of personal health data.
3. How might the integration of mental health services into primary healthcare change patient outcomes?
Answer:
Integrating mental health services into primary healthcare can lead to more comprehensive patient care and improved health outcomes by addressing both physical and mental health in a coordinated manner. This holistic approach ensures that mental health issues are identified and treated early, reducing the risk of more severe psychological problems and their associated physical health complications. By providing mental health support alongside routine medical care, patients are more likely to receive timely interventions and ongoing support, which can enhance their overall well-being and quality of life.
Additionally, the integration of mental health services can reduce stigma and improve access to care, as patients are more likely to seek help in a familiar primary care setting. It encourages a multidisciplinary approach to health, where healthcare providers collaborate to address all aspects of a patient’s health. Over time, this integrated model can lead to more effective management of chronic conditions, lower healthcare costs, and a healthier, more resilient population.
4. In what ways can public health campaigns drive behavioral changes that improve community health?
Answer:
Public health campaigns can drive significant behavioral changes by raising awareness about key health issues and promoting positive lifestyle choices. Effective campaigns use targeted messaging, community engagement, and multimedia outreach to educate the public on topics such as vaccination, nutrition, exercise, and disease prevention. By communicating clear and actionable information, these campaigns encourage individuals to adopt healthier behaviors and make informed decisions about their well-being, ultimately leading to improved community health outcomes.
Furthermore, public health campaigns often involve partnerships with community organizations, healthcare providers, and policymakers, which amplify their impact and foster a collective effort toward better health. These collaborations ensure that the messages reach a wide audience and are supported by accessible resources and services. The sustained effort of public health campaigns can result in long-term changes in social norms, reducing the prevalence of harmful behaviors and creating a more health-conscious society.
5. How might advancements in telemedicine reshape the accessibility of healthcare in remote areas?
Answer:
Advancements in telemedicine have the potential to dramatically reshape healthcare accessibility in remote and underserved areas by providing patients with immediate access to medical consultations and services regardless of geographic barriers. Telemedicine platforms allow patients to connect with healthcare providers through video calls, online chat, and remote monitoring devices, which is particularly beneficial in regions with limited medical infrastructure. This increased accessibility not only improves the timeliness of care but also reduces the need for costly and time-consuming travel to urban centers.
Additionally, telemedicine can facilitate continuous care through regular follow-ups and real-time monitoring, ensuring that patients receive consistent and comprehensive treatment. The use of digital tools in telemedicine also supports better management of chronic conditions and enables healthcare providers to deliver personalized care plans remotely. As telemedicine technologies continue to evolve, they promise to bridge the gap between urban and rural healthcare services, significantly improving health outcomes for populations in remote areas.
6. What ethical challenges arise with the increasing use of big data in healthcare?
Answer:
The increasing use of big data in healthcare brings several ethical challenges, particularly concerning privacy, consent, and data security. Collecting and analyzing large datasets often involves sensitive personal health information, which raises concerns about how this data is stored, shared, and used. There is a risk that without strict safeguards, patient confidentiality could be compromised, leading to unauthorized access or misuse of information. Furthermore, issues related to informed consent become more complex, as individuals may not fully understand how their data will be utilized in research and treatment.
In addressing these ethical challenges, it is essential to establish robust data protection policies and transparent practices that ensure patient information is used responsibly. Regulatory frameworks and international standards, such as GDPR, provide guidelines for data security and privacy, but continuous monitoring and enforcement are necessary to keep pace with technological advancements. Ethical considerations must remain at the forefront of healthcare innovation to maintain trust and ensure that the benefits of big data are realized without compromising individual rights.
7. How might global health crises, such as pandemics, influence the development of new healthcare policies and technologies?
Answer:
Global health crises, such as pandemics, have a profound impact on the development of new healthcare policies and technologies by exposing vulnerabilities in existing systems and prompting rapid innovation. These crises often lead to increased investment in healthcare infrastructure, digital health solutions, and emergency preparedness measures. Governments and healthcare organizations are compelled to adapt quickly by implementing policies that enhance surveillance, resource allocation, and public health responses, which can lead to lasting improvements in healthcare systems.
In response to pandemics, there is also a surge in the development and adoption of technologies such as telemedicine, remote monitoring, and data analytics, which facilitate efficient healthcare delivery under challenging circumstances. These advancements not only help manage the immediate crisis but also contribute to a more resilient healthcare system that is better prepared for future emergencies. The lessons learned from global health crises can drive long-term policy reforms and technological innovations that fundamentally transform healthcare delivery and improve population health.
8. In what ways can international collaboration enhance research and development in healthcare technology?
Answer:
International collaboration can significantly enhance research and development in healthcare technology by pooling resources, expertise, and diverse perspectives from across the globe. Collaborative efforts between research institutions, governments, and private companies can accelerate innovation by sharing data, conducting joint studies, and developing cutting-edge solutions to common healthcare challenges. This cooperative approach helps to overcome financial and technical barriers that individual entities might face, leading to breakthroughs in areas such as medical diagnostics, treatment modalities, and digital health platforms.
Moreover, international collaboration fosters a competitive yet supportive environment that drives continuous improvement and rapid advancements in healthcare technology. By working together, countries can establish common standards and regulatory frameworks that facilitate the global adoption of new technologies, ensuring that innovations are accessible and effective across diverse healthcare systems. This global network of collaboration not only accelerates the pace of technological development but also ensures that the benefits of innovation are distributed equitably, enhancing healthcare outcomes worldwide.
9. How might cultural factors influence the adoption and effectiveness of digital health solutions?
Answer:
Cultural factors play a significant role in the adoption and effectiveness of digital health solutions by shaping individuals’ attitudes toward technology and healthcare practices. In some cultures, there may be a high level of trust in traditional, face-to-face interactions with healthcare providers, which can slow the adoption of digital solutions. Conversely, cultures that are more tech-savvy and open to innovation may embrace digital health technologies more readily, leading to more effective integration and usage.
These cultural influences affect not only the initial acceptance of technology but also its long-term effectiveness in improving health outcomes. For digital health solutions to be successful, they must be designed with cultural sensitivity, ensuring that interfaces, language, and user experiences resonate with the target population. Tailoring digital health solutions to accommodate local cultural norms and preferences can enhance their usability, increase patient engagement, and ultimately lead to better healthcare delivery and outcomes.
10. What strategies can be employed to ensure data security and patient privacy in digital healthcare systems?
Answer:
Ensuring data security and patient privacy in digital healthcare systems requires a multi-layered approach that combines robust technical measures with stringent policy frameworks. Strategies include implementing strong encryption protocols, multi-factor authentication, and regular security audits to protect sensitive health data from unauthorized access. Additionally, clear privacy policies and consent processes must be established to ensure that patients are fully informed about how their data will be used and shared.
Governments and healthcare organizations should also invest in cybersecurity training for staff and continuously update their systems to defend against emerging threats. Collaboration with cybersecurity experts and adherence to international standards, such as the Health Insurance Portability and Accountability Act (HIPAA) or the General Data Protection Regulation (GDPR), further strengthen the security framework. By prioritizing these measures, digital healthcare systems can build trust among patients and ensure that their personal health information remains secure and confidential.
11. How can digital health platforms improve patient engagement and treatment adherence?
Answer:
Digital health platforms can improve patient engagement and treatment adherence by offering user-friendly interfaces, personalized health information, and interactive tools that encourage active participation in healthcare. These platforms provide reminders for medication, appointments, and health monitoring, which help patients stay on track with their treatment plans. Additionally, digital platforms often include features such as telehealth consultations, chat support, and educational resources, which empower patients to manage their health more effectively and make informed decisions.
The integration of gamification elements, such as rewards and progress tracking, can further motivate patients to adhere to treatment protocols. By offering real-time feedback and access to a supportive online community, digital health platforms create an environment where patients feel connected and accountable for their health outcomes. This comprehensive approach leads to higher levels of patient engagement, improved adherence to treatment, and ultimately better overall health outcomes.
12. How might the evolution of mobile health applications shape the future of patient care and preventive medicine?
Answer:
The evolution of mobile health applications is set to shape the future of patient care and preventive medicine by making health management more accessible, personalized, and proactive. Mobile apps allow individuals to monitor vital health parameters, receive personalized wellness tips, and access medical consultations remotely. This continuous monitoring can lead to early detection of health issues, timely interventions, and a shift towards preventive healthcare rather than reactive treatment. As mobile health technology advances, patients will increasingly rely on these tools for everyday health management, reducing the need for frequent in-person visits and lowering healthcare costs.
Furthermore, mobile health applications can facilitate the collection and analysis of large-scale health data, which can be used to inform public health strategies and personalized treatment plans. This data-driven approach enhances the ability of healthcare providers to track trends, predict outbreaks, and tailor interventions to specific populations. As a result, mobile health applications will play a critical role in advancing preventive medicine, improving patient outcomes, and transforming the overall healthcare landscape.
