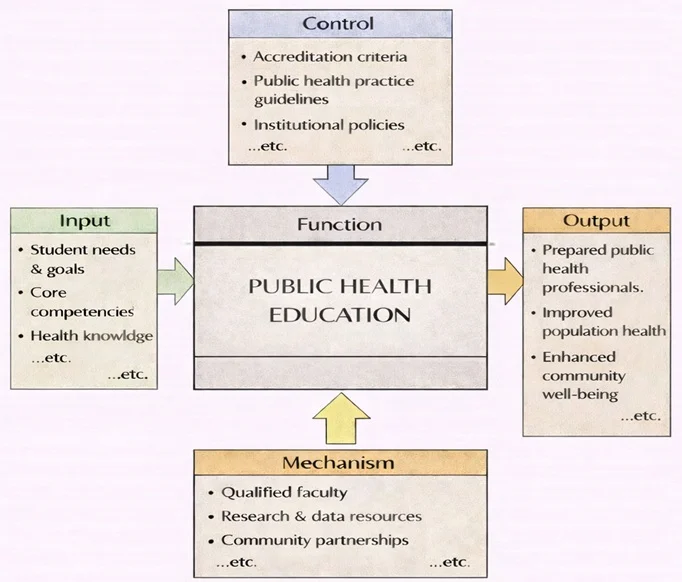
Public Health Education transforms student needs and learning goals into real capability for protecting and improving population health. Guided by accreditation requirements, public health practice guidelines, and institutional policies, it sets clear standards for what learners must know and be able to do. Using the right mechanisms—qualified faculty, research and data resources, and strong partnerships with communities and health agencies—this function connects classroom learning to real public health problems. The outputs are graduates prepared for public health roles, stronger prevention and response skills, and, ultimately, healthier and more resilient communities.
Public health is the science and practice of protecting and improving the health of populations through organized efforts, education, research, and policies. It focuses on preventing disease, prolonging life, and promoting health equity for all individuals, especially the most vulnerable. Unlike clinical medicine, which treats individual patients, public health addresses health issues on a community or societal level, emphasizing prevention over cure.
Public health integrates diverse fields such as epidemiology, environmental health, health policy, and behavioral sciences to understand and address complex health challenges. It aims to reduce health disparities, improve access to healthcare, and enhance the overall quality of life through sustainable interventions.

This colorful scene presents public health as a community-wide effort. A globe at the center symbolizes population health and global connections, while surrounding groups show everyday public health activities: clinic visits, health education, vaccination and screening, data monitoring, and support for families and older adults. Icons such as heart-rate symbols, medical crosses, charts, and laboratory items highlight surveillance, research, and evidence-based decision-making. Outdoor settings, clean-water and environment cues, and diverse people working together emphasize prevention and shared responsibility—improving wellbeing not just for individuals, but for whole communities.
Table of Contents
Focus of Public Health
The primary focus of public health is to prevent illness and promote health at the community, national, and global levels. It involves understanding the determinants of health—social, economic, and environmental factors—and implementing evidence-based strategies to address these determinants. Public health professionals collaborate with governments, non-profits, healthcare providers, and community organizations to design and implement programs that improve health outcomes.
Public health efforts range from controlling infectious diseases to addressing chronic conditions, ensuring clean water and air, and promoting healthy behaviors. The discipline emphasizes education, advocacy, and policy-making to create healthier environments and empower individuals to lead healthier lives.
Key Areas in Public Health
1. Epidemiology
- Definition: The study of the distribution and determinants of diseases and health conditions in populations.
- Key Functions:
- Monitoring disease patterns to identify outbreaks.
- Investigating causes and risk factors of diseases.
- Evaluating the effectiveness of public health interventions.
- Applications:
- Containing infectious diseases like COVID-19 through contact tracing and vaccination programs.
- Studying the rise of chronic conditions such as obesity and diabetes.
- Example Projects:
- Researching the link between smoking and lung cancer.
- Tracking seasonal influenza trends to predict outbreaks.
2. Health Policy and Management
- Definition: The development, implementation, and evaluation of policies to improve healthcare delivery and public health outcomes.
- Key Focus Areas:
- Designing healthcare systems that are efficient and equitable.
- Regulating healthcare costs and access.
- Addressing social determinants of health through policy.
- Applications:
- Formulating national vaccination strategies.
- Advocating for universal healthcare coverage.
- Examples:
- The Affordable Care Act in the United States, aimed at increasing healthcare access.
- Tobacco control policies to reduce smoking rates.
3. Community Health
- Definition: Focuses on improving health at the local level through education, resources, and preventive care.
- Key Activities:
- Conducting health awareness campaigns on topics like nutrition, exercise, and mental health.
- Implementing preventive screenings for conditions such as hypertension and cancer.
- Building partnerships with community organizations to address specific health needs.
- Applications:
- Reducing obesity through school-based wellness programs.
- Promoting breastfeeding in underserved communities to improve infant health.
Applications of Public Health
1. Managing Public Health Crises
- Overview:
Public health professionals are at the forefront of responding to crises such as pandemics, natural disasters, and bioterrorism threats. - Examples:
- Coordinating global efforts to control the COVID-19 pandemic through testing, treatment, and vaccination.
- Managing Ebola outbreaks by educating communities and implementing quarantine measures.
- Impact:
- Saving lives through rapid response and containment.
- Mitigating long-term health and economic impacts of crises.
2. Reducing Health Disparities
- Overview:
Public health seeks to eliminate disparities in health outcomes caused by socioeconomic, racial, or geographic inequalities. - Examples:
- Addressing food deserts in urban areas by promoting community gardens and healthy food access.
- Providing free or low-cost prenatal care to reduce maternal and infant mortality.
- Impact:
- Improving equity in health outcomes across diverse populations.
3. Disease Prevention and Control
- Overview:
Prevention is a cornerstone of public health, encompassing both communicable and non-communicable diseases. - Examples:
- Immunization programs to prevent diseases like measles and polio.
- Public campaigns to reduce smoking and promote physical activity.
- Impact:
- Reducing healthcare costs by preventing diseases before they occur.
4. Promoting Environmental Health
- Overview:
Public health addresses environmental factors that impact health, such as air quality, water safety, and climate change. - Examples:
- Regulating industrial emissions to reduce air pollution.
- Ensuring access to clean drinking water in rural areas.
- Impact:
- Protecting communities from environmental hazards.
Emerging Trends in Public Health
Digital Health and Telemedicine
- Leveraging technology to deliver health services and monitor populations remotely.
- Examples: Mobile health apps, wearable health monitors, and telehealth consultations.
Global Health Collaboration
- Strengthening international partnerships to address transnational health issues like pandemics and antibiotic resistance.
Focus on Mental Health
- Integrating mental health into primary healthcare to address the growing burden of mental illnesses.
Precision Public Health
- Using data analytics and genomics to target interventions more effectively.
Climate and Health
- Addressing the health impacts of climate change, such as heatwaves, vector-borne diseases, and food insecurity.
Challenges in Public Health
Resource Constraints
- Limited funding and resources, especially in low-income countries, hinder public health efforts.
Health Misinformation
- The spread of misinformation, particularly on social media, undermines public health campaigns.
Inequities in Access
- Socioeconomic and geographic barriers prevent equal access to healthcare services.
Emerging Diseases
- New and re-emerging infectious diseases pose ongoing threats to public health systems.
Future Directions in Public Health
Data-Driven Public Health
- Expanding the use of big data, AI, and machine learning to predict and address health trends.
Sustainable Health Systems
- Developing systems that are resilient to economic, environmental, and social changes.
Global Vaccination Initiatives
- Ensuring equitable distribution of vaccines for diseases like COVID-19, malaria, and tuberculosis.
Integration of Behavioral Sciences
- Incorporating behavioral insights to design more effective health interventions.
Why Study Public Health
Understanding the Health of Populations and Communities
Addressing Global Challenges with Evidence-Based Solutions
Promoting Health Equity and Social Justice
Developing Skills in Communication, Collaboration, and Policy
Preparing for a Wide Range of Health-Focused Careers
Public Health: Conclusion
Public health is essential for building healthier, more resilient communities. By focusing on prevention, education, and policy-making, it addresses the root causes of health challenges and strives to improve outcomes for all populations. Through advancements in technology, global collaboration, and innovative strategies, public health continues to evolve, tackling emerging issues while ensuring equitable access to healthcare. As societies face new and complex challenges, public health will remain at the forefront of efforts to protect and promote human well-being.
Frequently Asked Questions – Public Health
What is public health in simple terms?
Public health is the science and practice of protecting and improving the health of populations rather than focusing only on individual patients. It aims to prevent disease, extend life, and promote wellbeing through organised efforts such as vaccination, health education, policy, environmental protection, and community programmes.
How is public health different from clinical healthcare?
Clinical healthcare focuses on diagnosing and treating illness in individual patients, while public health focuses on preventing problems and improving health at community, national, or global levels. Public health professionals study patterns of disease, risks, and social conditions, then design policies and programmes to protect entire populations.
Why is public health important in today’s world?
Public health is vital for preventing outbreaks, managing pandemics, reducing the burden of chronic diseases, improving maternal and child health, addressing environmental risks, and tackling health inequalities. It helps societies use resources wisely and protect vulnerable groups, especially in a world that is highly connected and rapidly changing.
What kinds of topics and areas does public health cover?
Public health covers many areas, including epidemiology, biostatistics, environmental health, health promotion, health policy and management, global health, occupational health, maternal and child health, infectious disease control, and the social determinants of health such as housing, education, and income.
Which school subjects are useful preparation for studying public health at university?
Helpful subjects include biology and general science for understanding disease and the body, mathematics or statistics for working with data, and humanities or social sciences such as geography, economics, sociology, or history for understanding societies and inequalities. Languages and communication-based subjects are also valuable for working with diverse communities.
What skills and personal qualities are important for future public health professionals?
Public health professionals need analytical skills to interpret data, curiosity about how systems work, and clear communication skills to explain risks and recommendations. They also need teamwork, cultural sensitivity, ethical awareness, and persistence, because changing behaviour and policy often takes time and careful negotiation.
What do students typically learn in a public health degree or major?
Students usually learn epidemiology, biostatistics, health systems and policy, environmental and occupational health, global health, health promotion, research methods, and ethics. Many programmes also include case studies, projects with communities or agencies, and opportunities to explore topics such as nutrition, mental health, or infectious diseases in more depth.
What types of jobs and careers can public health graduates pursue?
Public health graduates can work in government health departments, hospitals and health systems, NGOs, international organisations, research institutes, community agencies, and private companies. Roles include epidemiologist, health promotion officer, policy analyst, programme coordinator, data analyst, community health worker, and health communications specialist.
How does public health address health inequalities and social determinants of health?
Public health recognises that health is shaped by social factors such as income, education, housing, employment, gender, and discrimination. It works to reduce inequalities by collecting evidence on who is most affected, designing targeted interventions, influencing policy, and partnering with communities to create fairer conditions for health.
How is data used in public health decision-making?
Public health relies heavily on data from sources such as surveillance systems, surveys, and health records. Professionals use this data to detect outbreaks, identify risk factors, evaluate programmes, and set priorities. Skills in analysing, interpreting, and communicating data are central to modern public health practice.
What is global health and how does it relate to public health?
Global health is a branch of public health that focuses on health issues that cross borders, such as pandemics, climate change, migration, and access to essential medicines. It emphasises cooperation between countries and organisations to improve health for all, especially in low-resource settings and marginalised populations.
How does the Public Health page on Prep4Uni.online support my study and career planning?
The Public Health page on Prep4Uni.online helps you see how biology, statistics, social sciences, and policy come together to improve population health. It introduces key concepts, links school subjects to university expectations, and gives you a clearer picture of the many career paths where you can combine data, policy, and community work to make a difference.
Public Health: Review Questions and Answers:
1. What is public health and why is it a critical field?
Answer: Public health is the science of protecting and improving the health of populations through education, policy making, and research for disease prevention. It focuses on the prevention of diseases and the promotion of healthy lifestyles across entire communities. This field plays a critical role in reducing health disparities and ensuring that communities have access to essential services and resources. By addressing social, economic, and environmental determinants of health, public health initiatives contribute to a safer, healthier, and more resilient society.
2. How do preventive care measures contribute to public health?
Answer: Preventive care measures are essential to public health as they focus on stopping diseases before they occur. These measures include vaccinations, health screenings, and health education programs that help identify risks early and reduce the burden of illness. They lead to improved quality of life by preventing chronic conditions and minimizing the need for expensive treatments. Preventive care also lowers healthcare costs and improves overall community well-being by ensuring early intervention and health maintenance.
3. What are some of the major challenges faced by public health professionals today?
Answer: Public health professionals face challenges such as emerging infectious diseases, chronic health conditions, and health disparities among different populations. They must also navigate the complexities of public policy, funding constraints, and global health threats that require coordinated international responses. Additionally, rapid technological changes and evolving social determinants of health add layers of complexity to public health initiatives. Addressing these challenges requires innovative strategies, effective collaboration, and ongoing research to develop sustainable solutions that benefit all communities.
4. How does public health policy influence community wellness?
Answer: Public health policy plays a significant role in shaping community wellness by establishing regulations and programs that protect health and prevent disease. These policies guide the allocation of resources, the implementation of preventive measures, and the development of health promotion campaigns. They also help create environments that support healthy behaviors, such as access to nutritious food, safe recreational spaces, and quality healthcare services. Through effective policy-making, public health initiatives can create lasting improvements in community health outcomes and reduce the prevalence of preventable diseases.
5. What is the role of education in advancing public health?
Answer: Education is fundamental to advancing public health as it empowers individuals with the knowledge needed to make informed decisions about their health. It promotes awareness about healthy practices, disease prevention, and the importance of regular health check-ups. Educational initiatives in public health also help to dispel myths and misinformation, fostering a culture of proactive health management. By integrating health education into schools, communities, and public campaigns, public health professionals can drive significant improvements in overall societal well-being.
6. How do social determinants impact public health outcomes?
Answer: Social determinants such as income, education, employment, and housing have a profound impact on public health outcomes by influencing an individual’s access to resources and opportunities for healthy living. These factors can determine the prevalence of chronic diseases, life expectancy, and overall quality of life within communities. Public health initiatives aim to address these underlying determinants by implementing policies that promote equity and reduce disparities. By improving social conditions, public health efforts can significantly enhance the health and well-being of entire populations.
7. What role does research play in shaping public health interventions?
Answer: Research is at the core of public health interventions as it provides the evidence needed to develop effective strategies for disease prevention and health promotion. It involves the systematic study of health trends, risk factors, and the effectiveness of various interventions, which in turn informs policy decisions and program development. Through rigorous scientific investigation, public health research identifies the best practices and innovative solutions that can be scaled up to benefit larger populations. This research-driven approach ensures that public health initiatives are both evidence-based and adaptive to emerging challenges.
8. How can technology improve public health surveillance and response?
Answer: Technology improves public health surveillance and response by enabling the rapid collection, analysis, and dissemination of health data. Digital tools such as electronic health records, mobile health applications, and data analytics platforms facilitate real-time monitoring of disease outbreaks and health trends. These technological advancements allow public health officials to identify potential threats quickly and implement timely interventions. Enhanced surveillance systems ultimately lead to more efficient responses, better resource allocation, and improved overall public health outcomes.
9. What strategies can be implemented to reduce health disparities in vulnerable populations?
Answer: Strategies to reduce health disparities in vulnerable populations include targeted interventions such as community health programs, improved access to healthcare services, and culturally tailored health education initiatives. These strategies address the unique challenges faced by marginalized groups by providing resources and support that are specifically designed to meet their needs. Additionally, policy reforms and increased funding for public health initiatives can help bridge the gap in healthcare access and quality. By focusing on equity and social determinants of health, public health efforts can significantly improve outcomes for vulnerable populations.
10. How does global collaboration contribute to addressing international public health challenges?
Answer: Global collaboration contributes to addressing international public health challenges by fostering the exchange of knowledge, resources, and best practices among countries. It enables coordinated efforts to tackle issues such as pandemics, chronic diseases, and environmental health threats that transcend national borders. Collaborative international initiatives facilitate the development of standardized protocols, joint research projects, and shared responses to emerging health crises. Such cooperation is essential for creating a unified and effective global public health system that can adapt to and mitigate widespread health threats.
Public Health: Thought-Provoking Questions and Answers
1. How might emerging digital health technologies transform the future of public health surveillance and intervention?
Answer:
Emerging digital health technologies, including real-time data analytics, wearable devices, and mobile health applications, are set to revolutionize public health surveillance by enabling continuous, real-time monitoring of population health trends. These technologies can collect vast amounts of health-related data from diverse sources, allowing for the early detection of outbreaks and emerging health threats. With advanced analytics, public health officials can quickly identify patterns and respond with targeted interventions, potentially curbing the spread of diseases before they escalate into epidemics. The integration of these digital tools into public health systems promises a more proactive, efficient, and data-driven approach to health management, ultimately leading to better health outcomes on a global scale.
Furthermore, digital health technologies can enhance communication between healthcare providers, policymakers, and the public, ensuring that critical information is disseminated quickly and effectively during health emergencies. They also facilitate the collection of personalized health data, which can inform more tailored public health interventions. As these technologies continue to evolve, they are likely to reshape the way public health is practiced, making it more responsive, precise, and collaborative.
2. In what ways can public-private partnerships enhance global public health initiatives?
Answer:
Public-private partnerships can significantly enhance global public health initiatives by combining the strengths of both sectors to address complex health challenges. Private companies often bring innovation, advanced technology, and substantial financial resources, while public agencies provide regulatory oversight, broad reach, and policy support. Together, these partnerships can develop and implement large-scale health programs that effectively target issues such as disease prevention, vaccination campaigns, and health education. By leveraging the expertise and resources of both sectors, public-private partnerships can create more sustainable and impactful public health interventions that benefit communities worldwide.
Moreover, these collaborations foster innovation by encouraging the sharing of best practices and the development of new technologies tailored to public health needs. They can also streamline the implementation of health initiatives by reducing bureaucratic obstacles and improving resource allocation. The success of public-private partnerships in global public health hinges on clear communication, mutual trust, and a shared commitment to improving health outcomes, making them an essential component of modern health strategies.
3. How might climate change impact public health, and what measures can be taken to mitigate these effects?
Answer:
Climate change has far-reaching impacts on public health, including increased rates of respiratory illnesses, heat-related conditions, and vector-borne diseases. Rising temperatures and extreme weather events can exacerbate pollution levels and create environments conducive to the spread of infectious diseases, posing significant challenges to global health. To mitigate these effects, public health initiatives must incorporate strategies that focus on both adaptation and prevention. This includes improving infrastructure to withstand extreme weather, enhancing early warning systems, and promoting sustainable practices that reduce greenhouse gas emissions.
Additionally, public health policies should prioritize community education and preparedness, ensuring that vulnerable populations are informed and equipped to cope with climate-related health risks. Collaborative efforts between governments, non-governmental organizations, and international agencies are crucial for developing comprehensive strategies that address both the immediate and long-term health impacts of climate change. By taking proactive measures, public health systems can better protect communities and reduce the adverse effects of environmental changes on human health.
4. What role does health literacy play in improving public health outcomes, and how can it be promoted?
Answer:
Health literacy is fundamental to improving public health outcomes as it empowers individuals to understand, process, and act on health information. Higher health literacy leads to better decision-making regarding personal health, more effective management of chronic conditions, and greater adherence to preventive care measures. When individuals are well-informed about health risks and the benefits of healthy behaviors, they are more likely to engage in proactive health management, leading to improved overall well-being. To promote health literacy, public health initiatives can include educational campaigns, community workshops, and digital resources that simplify complex health information into accessible, actionable content.
Enhancing health literacy also involves fostering partnerships between healthcare providers, educators, and community leaders to ensure that information is culturally appropriate and tailored to the needs of diverse populations. By integrating health education into schools and community programs, public health authorities can build a foundation of knowledge that supports lifelong health. This comprehensive approach not only improves individual outcomes but also strengthens the overall public health infrastructure, contributing to healthier communities.
5. How can the integration of behavioral science principles into public health campaigns improve their effectiveness?
Answer:
The integration of behavioral science principles into public health campaigns can significantly improve their effectiveness by addressing the underlying psychological factors that influence health-related behaviors. Behavioral science offers insights into how people make decisions, the impact of social norms, and the barriers to behavior change. By applying these principles, public health campaigns can be designed to motivate individuals, overcome resistance to change, and promote healthier habits. Techniques such as nudging, framing, and incentive-based interventions can encourage people to adopt positive health behaviors, such as regular exercise, vaccination, and healthy eating.
Furthermore, behavioral science can inform the design of messages that resonate with target audiences, ensuring that public health communications are both persuasive and culturally sensitive. By tailoring campaigns to address specific cognitive biases and motivational factors, public health authorities can enhance engagement and drive sustained behavioral change. The result is a more effective public health strategy that not only increases awareness but also leads to measurable improvements in community health outcomes.
6. What potential impacts could emerging infectious diseases have on global public health, and how should systems prepare?
Answer:
Emerging infectious diseases can have profound impacts on global public health by triggering widespread outbreaks, overwhelming healthcare systems, and causing significant economic and social disruption. These diseases often spread rapidly due to global travel and interconnected populations, posing challenges in containment and management. To prepare for such threats, public health systems must invest in robust surveillance networks, rapid response protocols, and flexible healthcare infrastructure. Early detection and effective intervention are critical for mitigating the spread and impact of infectious diseases.
In addition, international collaboration and data sharing are essential for coordinating responses and developing effective treatments and vaccines. Governments and health organizations should focus on building resilient systems that can quickly adapt to emerging challenges through continuous monitoring, research, and public education campaigns. Strengthening these capabilities not only protects public health but also enhances global readiness for future pandemics, ensuring a more coordinated and effective response.
7. How might public health policies evolve in response to an aging global population?
Answer:
Public health policies are likely to evolve significantly in response to an aging global population by focusing on the unique healthcare needs of older adults. These policies may prioritize preventive care, chronic disease management, and geriatric services to improve the quality of life for seniors. As life expectancy increases, there is a growing need for healthcare systems to support long-term care, social integration, and mental health services for older populations. Policies may also emphasize the development of age-friendly communities, including accessible transportation, safe housing, and community-based health programs that cater to the elderly.
Additionally, public health strategies will need to address the economic and social implications of an aging population, such as increased healthcare costs and potential workforce shortages. This could involve incentivizing preventive measures and promoting healthy aging through education and wellness programs. As a result, the evolution of public health policies will be crucial in ensuring that healthcare systems remain sustainable and capable of meeting the needs of an aging society, ultimately contributing to overall societal well-being.
8. What role does environmental health play in shaping public health initiatives, and how can it be addressed?
Answer:
Environmental health plays a critical role in shaping public health initiatives by addressing the impacts of environmental factors on human health. Issues such as air and water pollution, chemical exposures, and climate change can have significant adverse effects on population health. Public health initiatives must therefore incorporate environmental health strategies that aim to reduce exposure to harmful substances, promote clean energy, and ensure safe living conditions. These strategies often involve regulatory measures, community education, and coordinated efforts among government agencies and environmental organizations.
Addressing environmental health requires a multifaceted approach that includes rigorous monitoring, policy enforcement, and public engagement. By integrating environmental health into public health planning, authorities can implement preventive measures that reduce the incidence of diseases related to environmental hazards. This holistic approach not only improves individual health outcomes but also fosters a healthier and more sustainable environment for future generations.
9. How can public health systems leverage global data to improve health outcomes at the community level?
Answer:
Public health systems can leverage global data to improve community health outcomes by analyzing international health trends, disease surveillance data, and demographic statistics to inform local health strategies. Access to global datasets allows health authorities to identify emerging health threats and benchmark community performance against international standards. This data-driven approach enables targeted interventions and resource allocation that address specific health challenges within communities. By integrating global data into local public health planning, policymakers can develop evidence-based programs that improve health outcomes and enhance community resilience.
Furthermore, global data facilitates international collaboration and knowledge sharing, which can lead to the adoption of best practices and innovative solutions from other regions. This collaborative exchange of information supports the development of comprehensive health policies that are both proactive and adaptive. Ultimately, the strategic use of global data in public health systems not only improves individual health outcomes but also strengthens the overall health infrastructure at the community level.
10. How might the rise of health misinformation on digital platforms impact public health, and what strategies can be implemented to combat it?
Answer:
The rise of health misinformation on digital platforms poses significant challenges to public health by potentially spreading false information that undermines effective healthcare practices and public trust. Misinformation can lead to vaccine hesitancy, improper self-medication, and resistance to public health guidelines, which in turn can exacerbate health crises. To combat this, public health systems must implement robust strategies that include fact-checking, digital literacy programs, and proactive communication campaigns designed to dispel myths and provide accurate, evidence-based information. Collaboration with social media companies and influencers can also help amplify credible sources and counteract the spread of false narratives.
Moreover, enhancing community engagement and establishing transparent communication channels are essential for building public trust. Educating the public on how to critically evaluate health information online empowers individuals to make informed decisions. By addressing health misinformation through a multifaceted approach, public health authorities can mitigate its negative impacts and promote a more informed and resilient society.
11. How can public health initiatives address the social determinants of health to improve overall community well-being?
Answer:
Public health initiatives can address the social determinants of health by implementing policies and programs that target the underlying social, economic, and environmental factors affecting health outcomes. This involves improving access to education, housing, and employment opportunities, which are critical for promoting health equity and reducing disparities. By focusing on these determinants, public health efforts can create more supportive environments that facilitate healthy behaviors and reduce the incidence of chronic diseases. Additionally, collaborative community-based programs and partnerships with local organizations can help tailor interventions to meet the unique needs of different populations.
Addressing social determinants requires a comprehensive, multi-sectoral approach that integrates health, social services, and policy reforms. Initiatives such as improving neighborhood safety, increasing access to nutritious foods, and enhancing healthcare services in underserved areas contribute significantly to overall community well-being. By creating environments that support healthy living, public health initiatives can lead to long-term improvements in population health and foster a more equitable society.
12. What future trends might shape the evolution of public health, and how should systems prepare for them?
Answer:
Future trends that might shape the evolution of public health include advancements in digital health technologies, increased focus on personalized and preventive care, and the growing impact of climate change on health. The integration of artificial intelligence, big data, and telemedicine is likely to transform how public health surveillance, diagnosis, and intervention are conducted. Additionally, emerging global health challenges such as pandemics and chronic diseases will require more adaptive and responsive public health systems that can address both individual and community needs.
To prepare for these future trends, public health systems must invest in technology, infrastructure, and workforce training. Building resilient healthcare networks that incorporate advanced data analytics and digital communication tools is essential for timely responses to health crises. Furthermore, fostering interdisciplinary collaboration and continuous research will help ensure that public health policies remain evidence-based and forward-thinking. By proactively addressing these emerging trends, public health systems can improve their capacity to promote long-term health and well-being for diverse populations.
